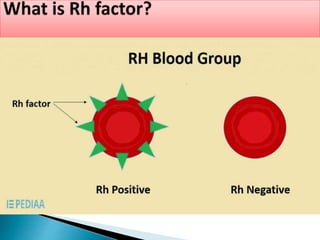
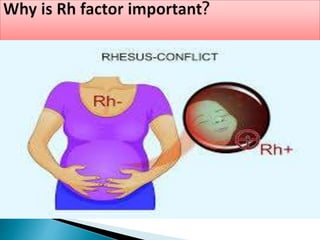
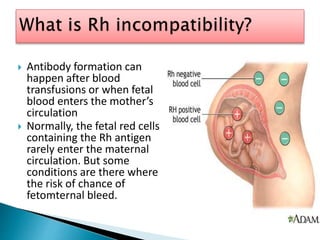
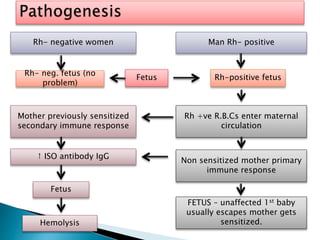
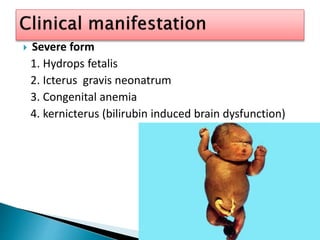
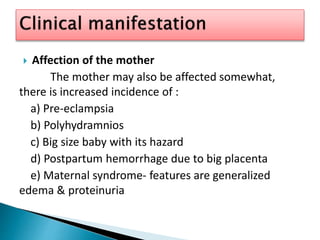
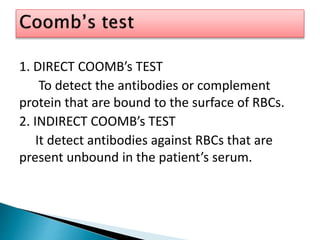
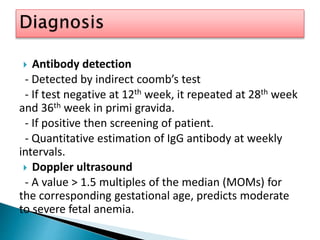
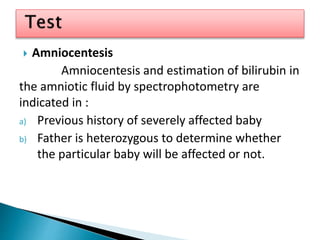
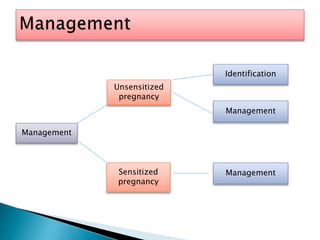
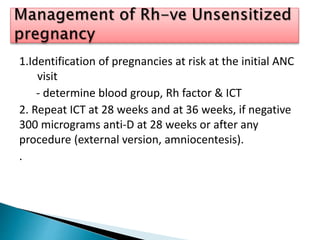
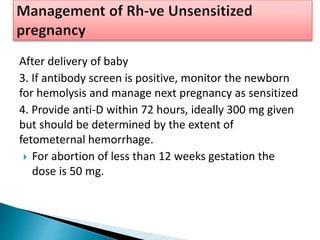
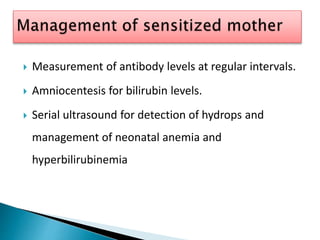
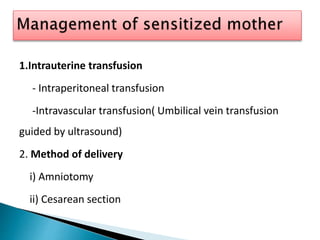
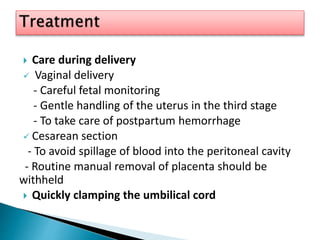
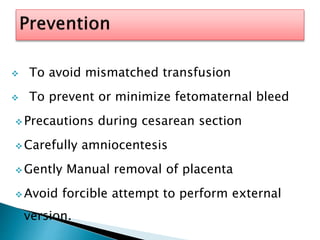
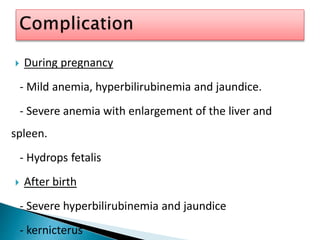
Rh-incompatibility occurs when a mother has Rh-negative blood type and the fetus has Rh-positive blood type. This can lead to complications in pregnancy if the fetus' red blood cells enter the mother's circulation and cause her to form antibodies. Management involves identifying at-risk pregnancies, monitoring antibody levels, and providing RhIg injections as prophylaxis. For sensitized pregnancies, careful fetal monitoring and interventions like intrauterine transfusions or early delivery may be needed to prevent complications in the fetus like hydrops fetalis.