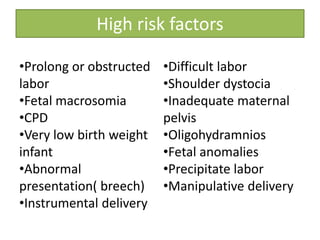
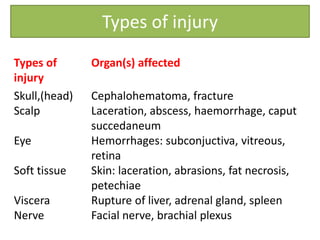
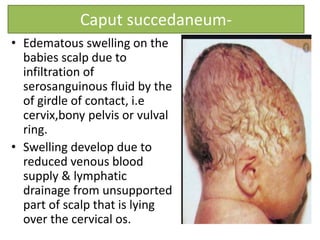
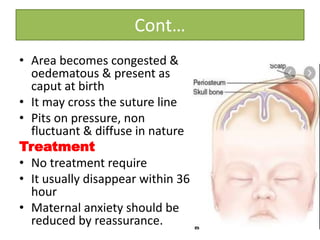
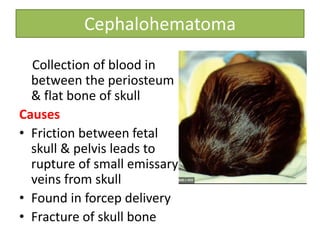
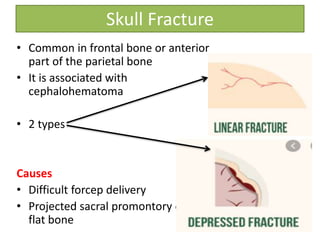
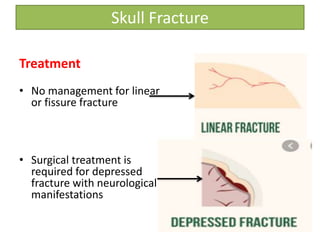
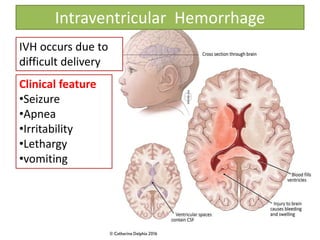
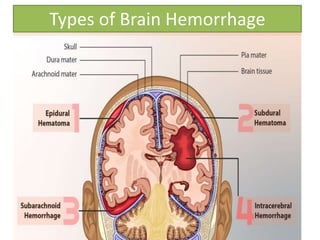
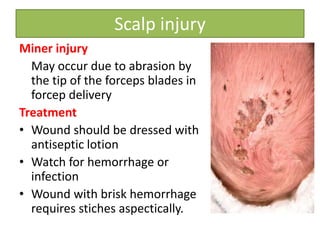
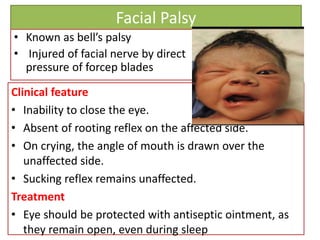
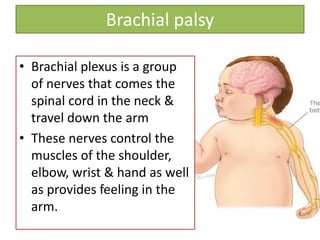
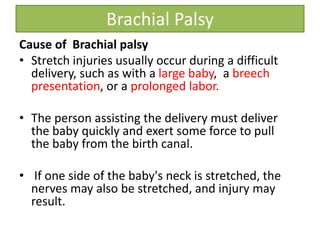
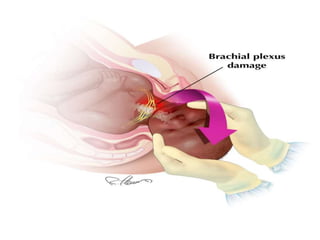
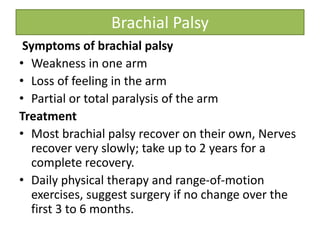
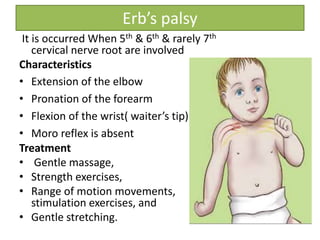
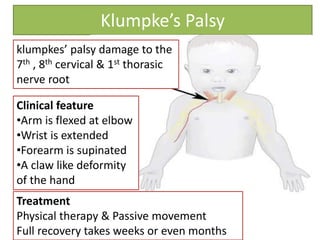
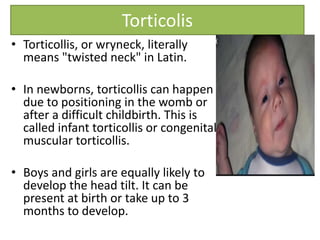
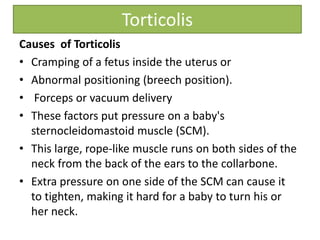
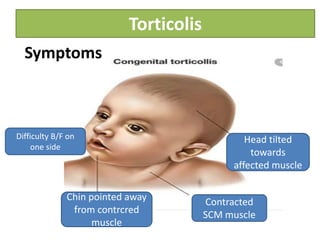
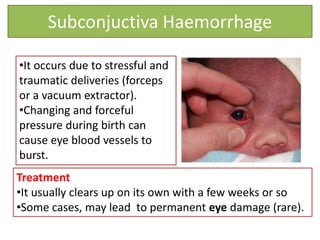
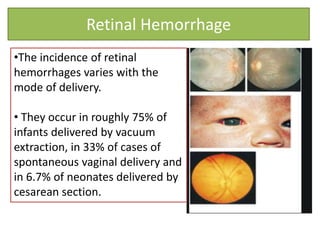
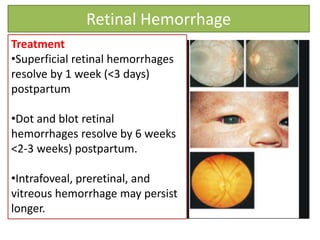
This document discusses birth injuries, including their definition, risk factors, types, symptoms, treatment and prevention. It defines birth injury as impairment of the infant's body function or structure due to adverse influences during birth. Common types of injuries discussed include skull or head injuries (cephalohematoma, fractures), facial or nerve injuries (facial palsy, brachial plexus injuries), and soft tissue injuries (subconjunctival hemorrhages, retinal hemorrhages). Prevention strategies include proper prenatal care, monitoring for fetal distress, recognizing when c-section is necessary, and careful delivery techniques.