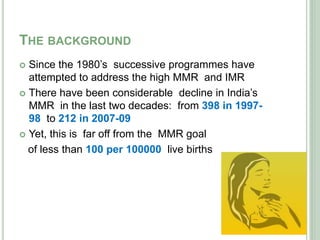
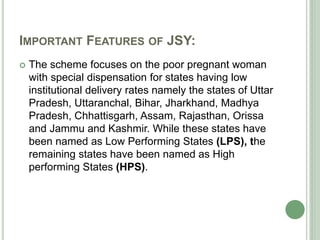
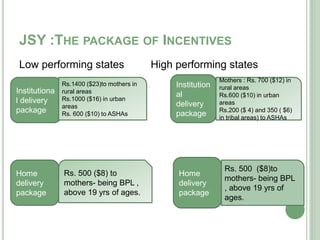
This document discusses the importance of institutional deliveries in India. It notes that India has high maternal and child mortality rates. Institutional deliveries, where birth takes place at a medical facility with trained staff, can help reduce these rates by providing proper medical care and addressing complications. However, utilization of institutional delivery services remains low in India due to various socioeconomic barriers like poverty, lack of education, and distance from health facilities. The National Rural Health Mission and Janani Suraksha Yojana aim to increase institutional deliveries among poor women through cash incentives and improving access to healthcare.