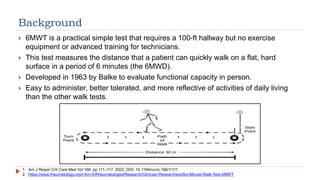
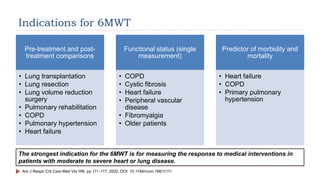
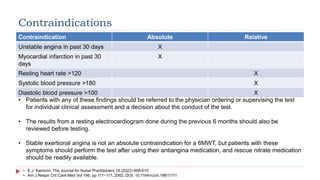
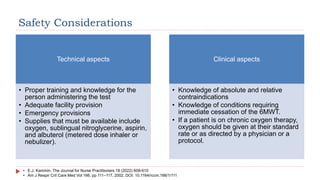
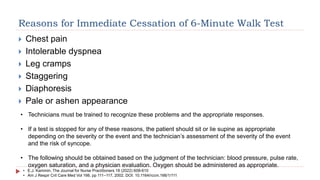
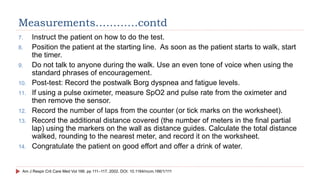
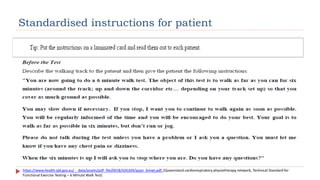
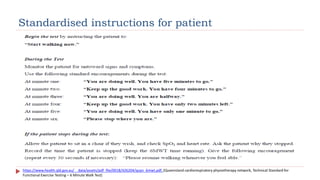
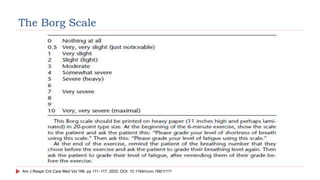
The 6-minute walk test (6MWT) measures the distance a patient can walk in 6 minutes on a flat, hard surface. It was developed in 1963 to evaluate functional capacity. It is a simple test that requires only a 100-foot hallway. The 6MWT evaluates the integrated responses of the pulmonary, cardiovascular, and muscular systems during exercise. It is commonly used to assess responses to treatments for heart and lung diseases and to predict morbidity and mortality. The test must be administered according to strict protocols and has contraindications for patients with unstable medical conditions.