The document provides an overview of the basics of anesthesia, including:
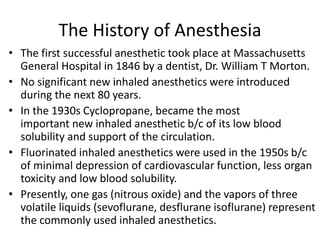
- A brief history of anesthesia from the first successful anesthetic in 1846 to modern inhaled anesthetics.
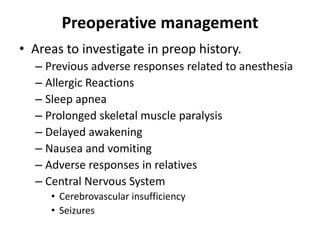
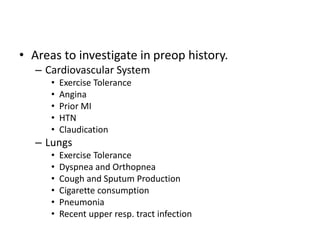
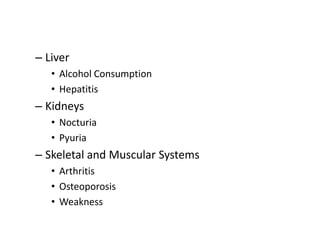
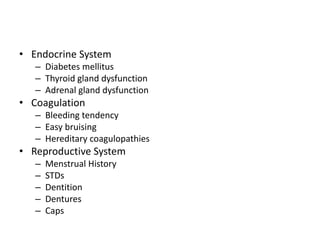
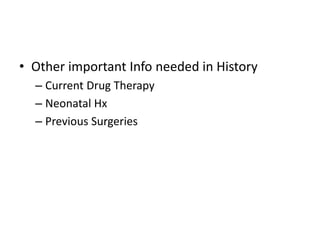
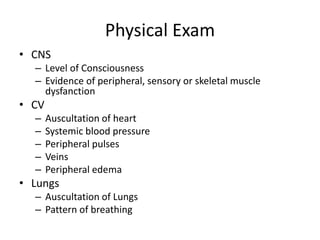
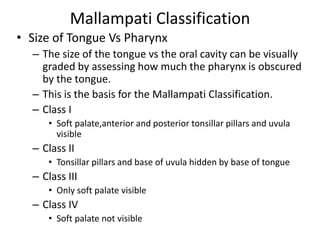
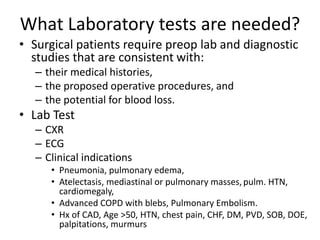
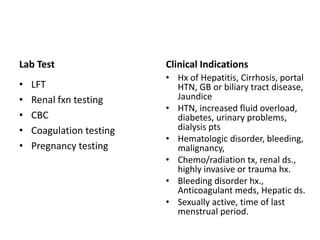
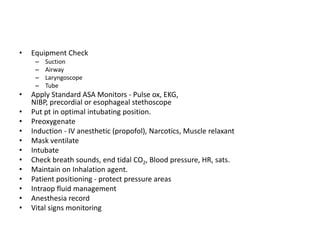
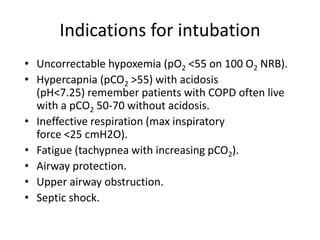
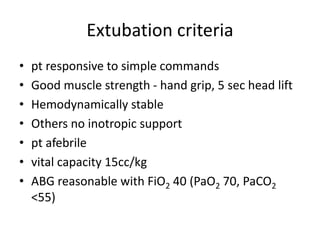
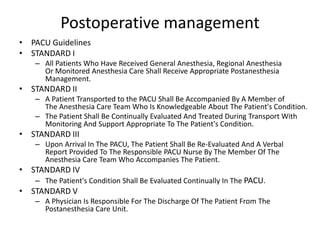
- Details on preoperative, intraoperative, and postoperative patient management, including assessments, monitoring, intubation/extubation criteria.
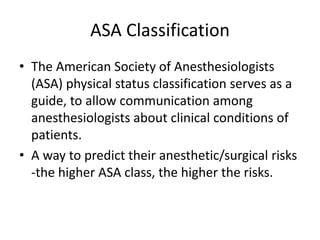
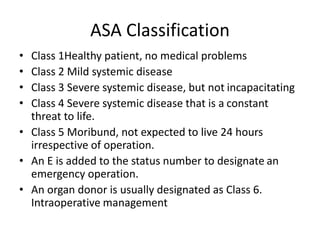
- Choices of anesthesia like general, regional, monitored or local anesthesia and ASA classifications to predict risks.
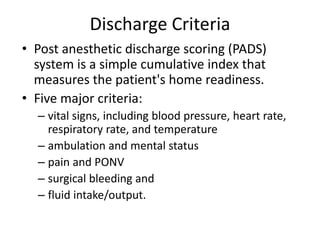
- Postoperative guidelines focus on evaluating patient status and readiness for discharge using a post anesthetic discharge scoring system.