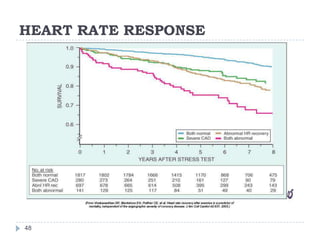
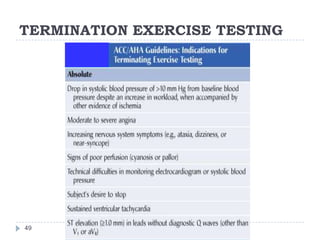
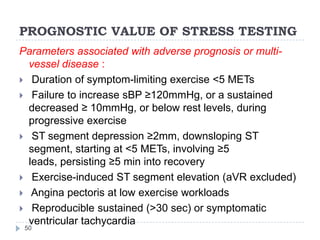
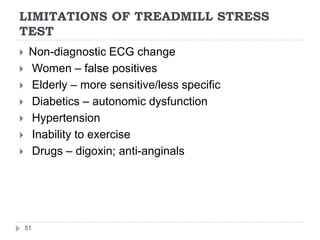
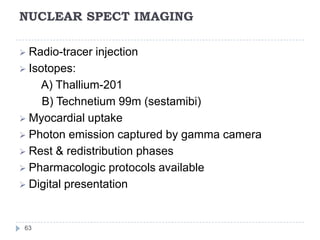
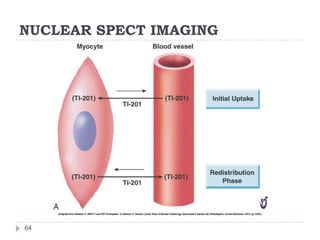
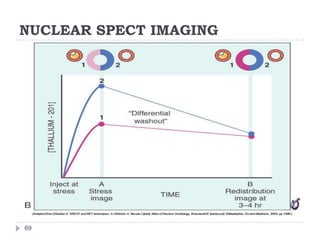
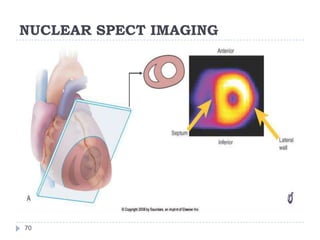
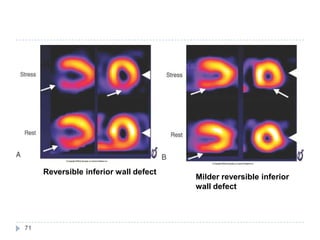
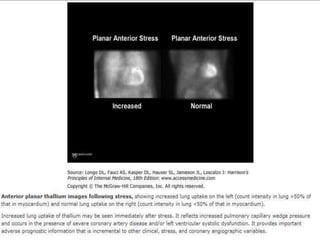
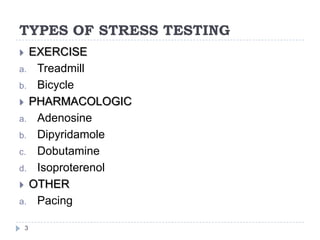
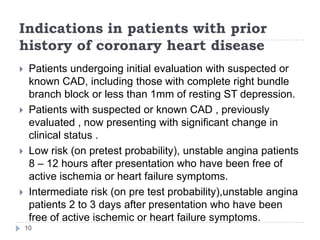
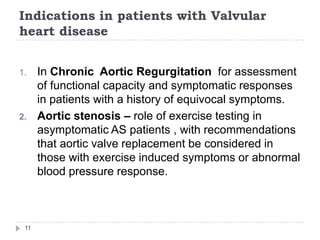
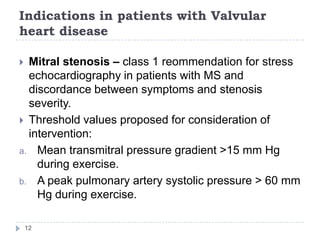
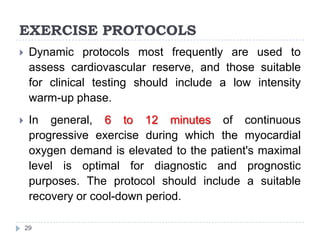
This document discusses stress testing, which measures the heart's response to external stress. There are two main types of stress testing - exercise testing using treadmills or bicycles, and pharmacological testing using medications. Stress testing can help diagnose coronary artery disease, evaluate functional capacity, and assess treatment effects. The document outlines guidelines for indications, contraindications, and interpretations of different stress test results. Key measurements taken during stress tests include ECG, exercise capacity, symptoms, blood pressure, and heart rate response.

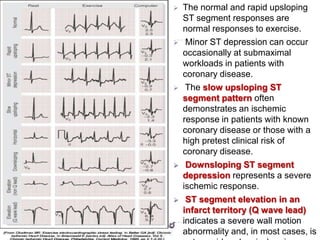
![39
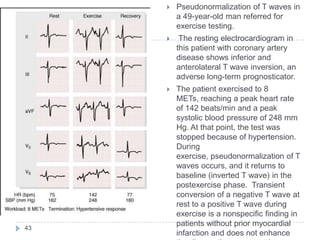
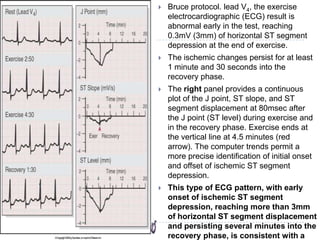
A 48-year-old man with
several atherosclerotic risk
factors and a normal resting
electrocardiographic (ECG)
result, developed marked ST
segment elevation (4 mm
[arrows]) in leads V2 and V3
with lesser degrees of ST
segment elevation in leads
V1 and V4 and J point
depression with upsloping
ST segments in lead
II, associated with angina.
This type of ECG pattern is
usually associated with a
full-thickness, reversible
myocardial perfusion defect
in the corresponding left
ventricular myocardial
segments and high-grade
intraluminal narrowing at
coronary angiography.](https://image.slidesharecdn.com/stresstestingseminar-130726094716-phpapp01/85/Stress-Testing-39-320.jpg)