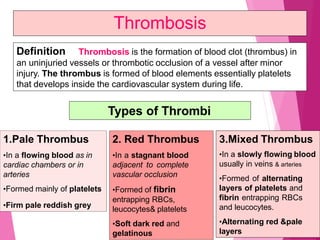
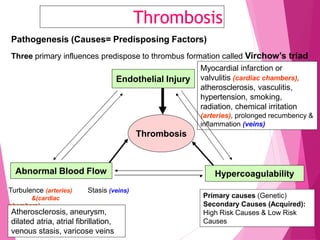
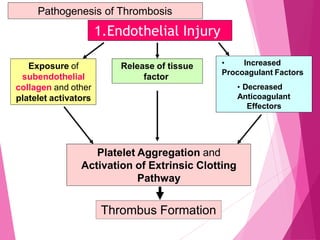
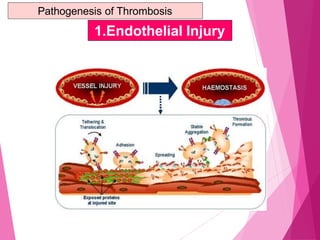
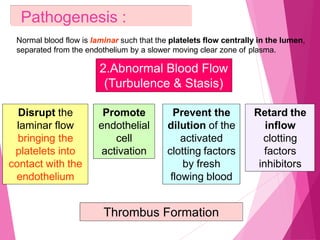
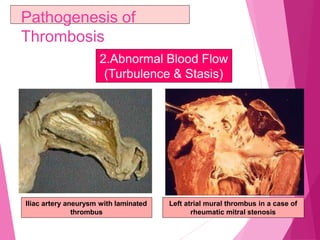
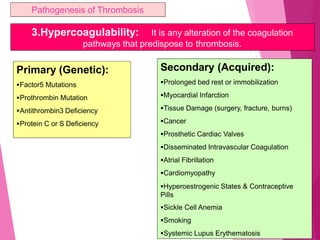
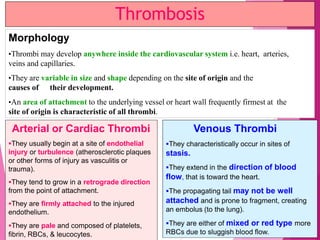
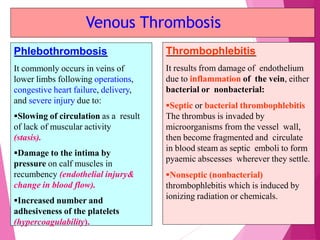
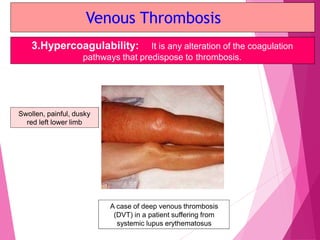
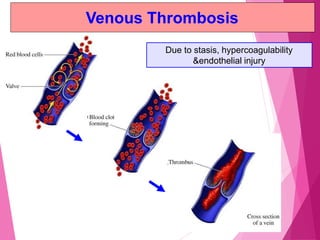
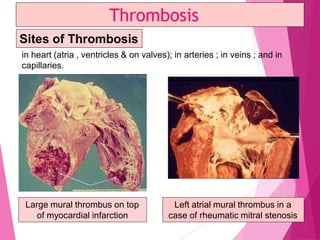
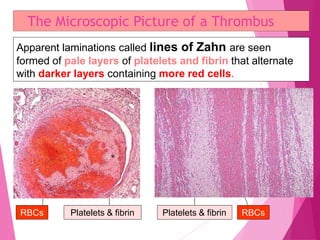
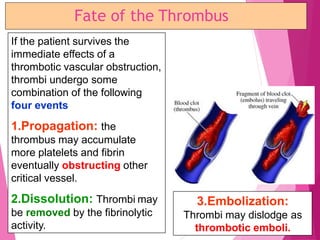
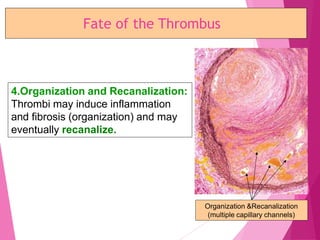
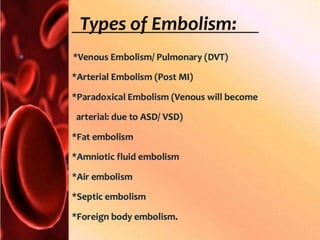
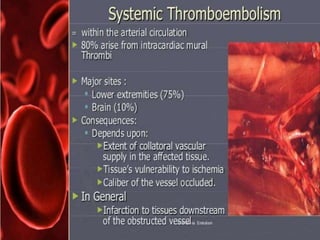
Thrombosis is the formation of a blood clot (thrombus) inside a blood vessel or heart chamber. There are three main types of thrombi based on composition and location. Thrombosis occurs due to endothelial injury, abnormal blood flow, and hypercoagulability. Thrombi form at sites of injury or turbulence in arteries and heart chambers, and at sites of stasis in veins. Microscopically, thrombi appear laminated with alternating pale and dark layers. Thrombosis can occur in any blood vessel and lead to complications such as embolism if parts of the thrombus break off.