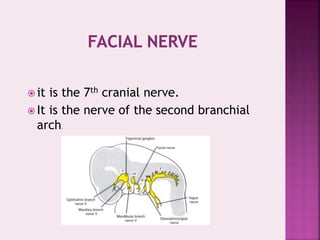
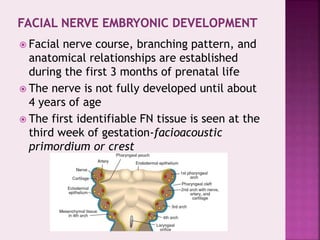
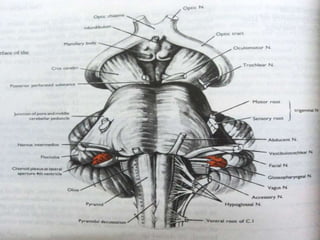
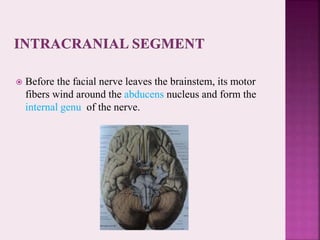
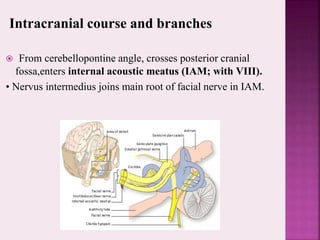
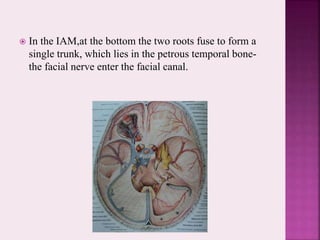
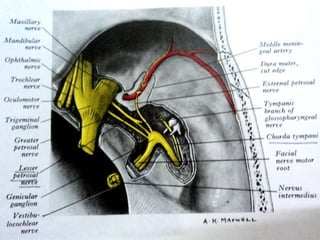
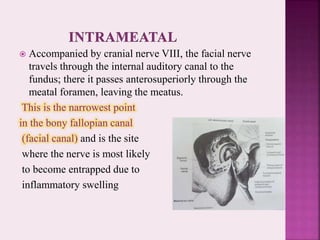
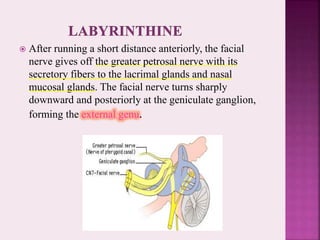
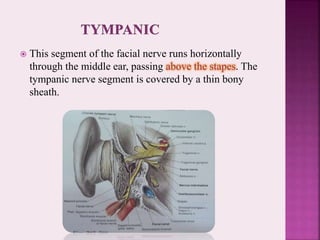
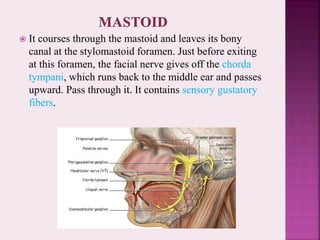
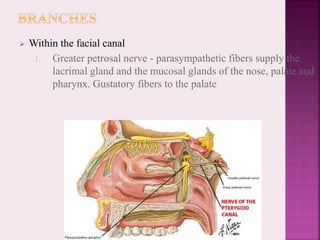
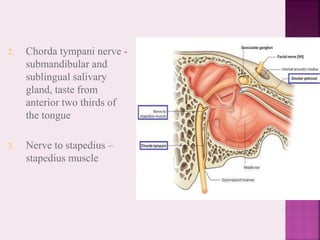
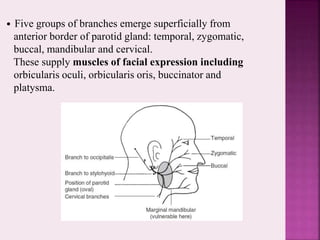
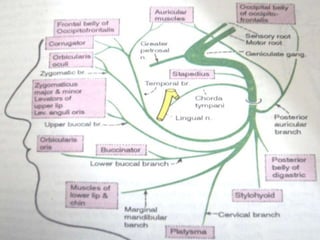
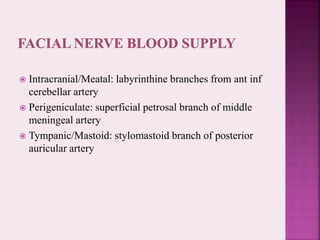
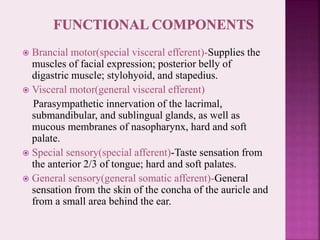
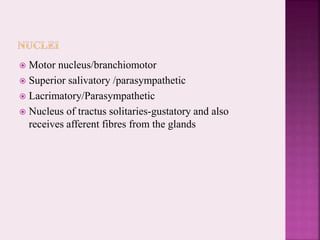
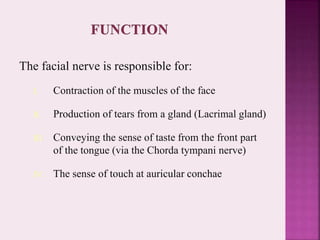
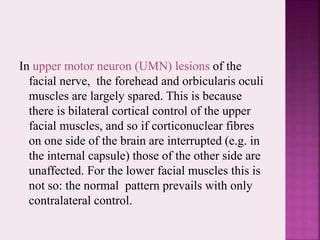
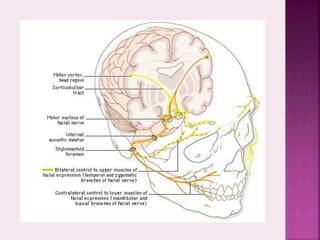
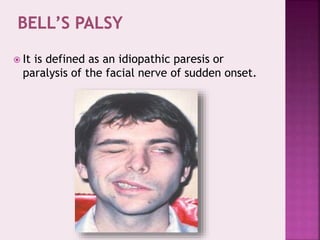
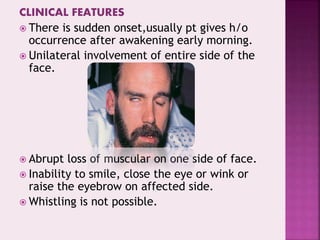
The facial nerve (CN VII) is responsible for facial muscle movement and taste. It originates in the brainstem and travels through the facial canal in the temporal bone. The main branches innervate the muscles of facial expression. Facial paralysis can occur from lesions at different levels and have varying clinical presentations. Bell's palsy is an idiopathic acute facial paralysis that usually resolves over time with treatment. Evaluation and management depends on the severity and cause of injury.