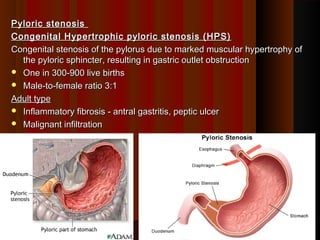
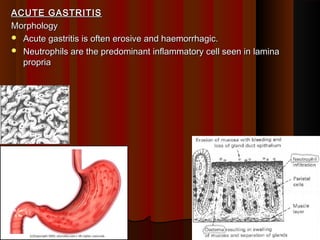
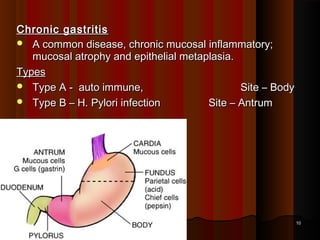
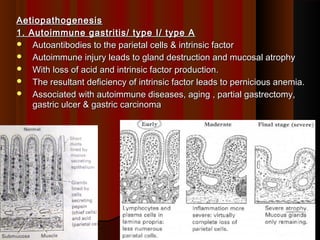
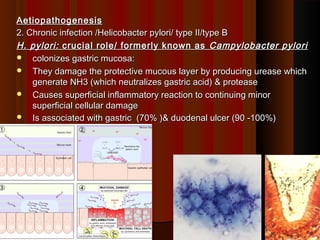
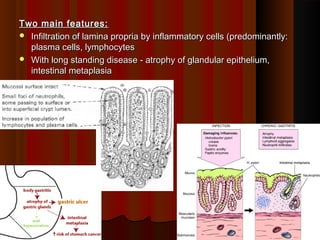
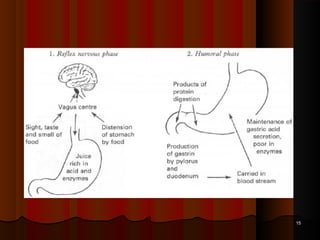
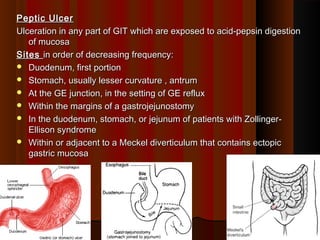
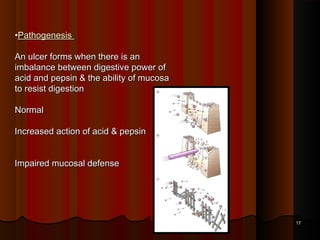
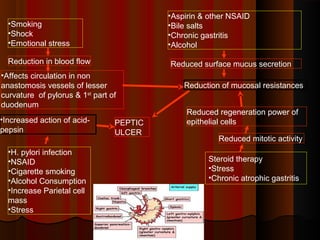
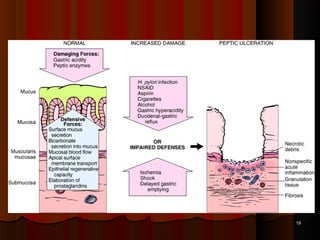
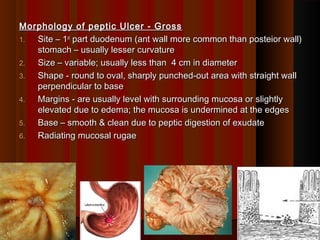
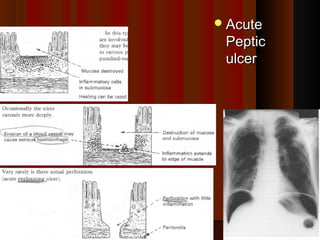
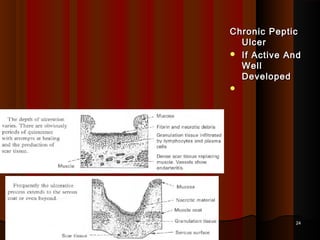
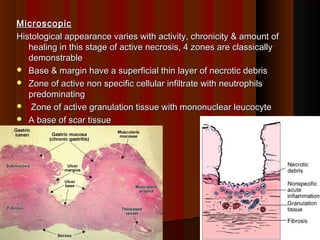
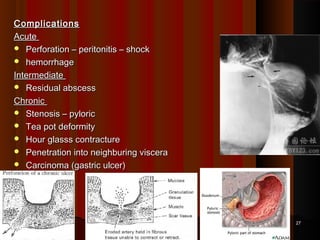
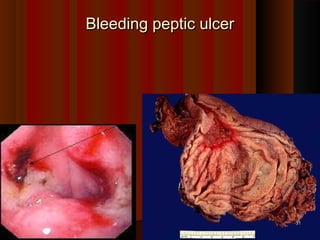
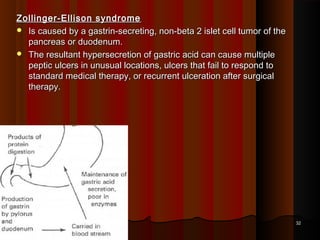
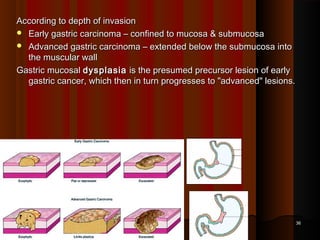
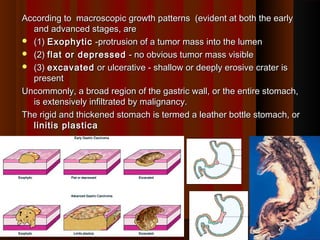
This document discusses various gastrointestinal conditions including pyloric stenosis, gastritis, peptic ulcer, and gastric tumors. It defines each condition and describes their causes, characteristics, pathogenesis, clinical presentation, treatment and complications. Pyloric stenosis is a congenital narrowing of the pylorus. Gastritis is inflammation of the gastric mucosa which can be acute or chronic. Peptic ulcer is an erosion in the gastrointestinal tract exposed to acid and pepsin digestion. Gastric tumors can be benign or malignant and include adenocarcinoma as a common malignant tumor type. Risk factors discussed include H. pylori infection, smoking, diet, and genetic conditions.