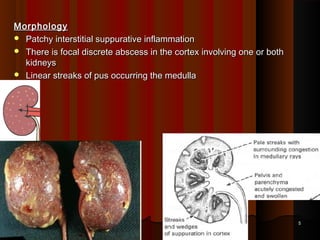
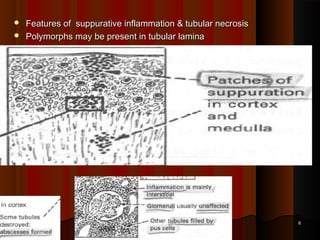
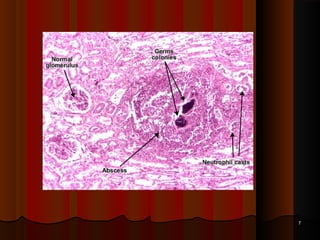
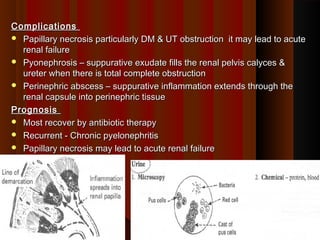
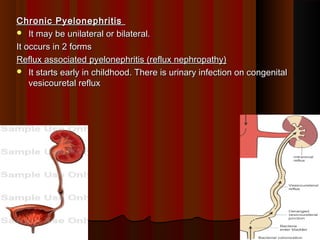
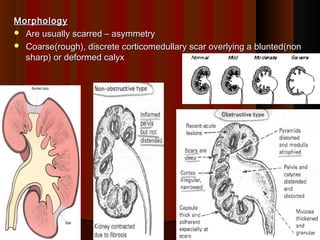
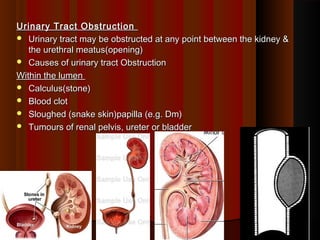
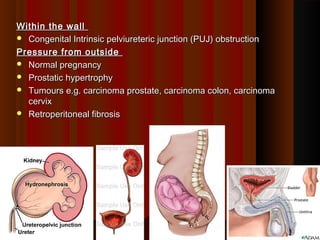
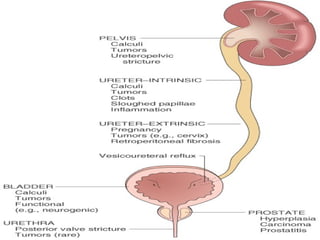
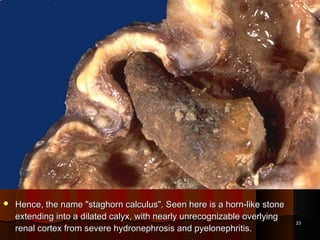
UTIs are grouped as pyelonephritis (inflammation of the renal pelvis, tubules, and interstitium) or cystitis (inflammation of the urinary bladder). The most common causes of UTIs are endogenous bacteria like E. coli, which cause 75-90% of infections. Risk factors include urinary obstruction, pregnancy, vesicoureteral reflux, diabetes, and instrumentation. Complications can include renal abscesses, pyonephrosis if the kidney is completely obstructed, and acute renal failure. Chronic pyelonephritis may cause scarred and deformed kidneys.