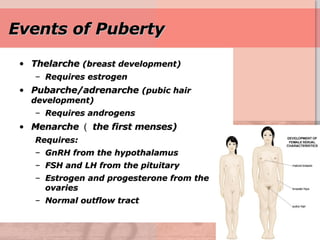
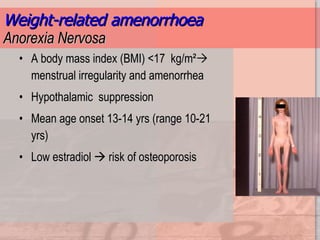
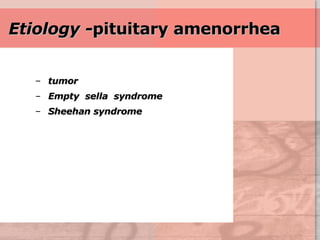
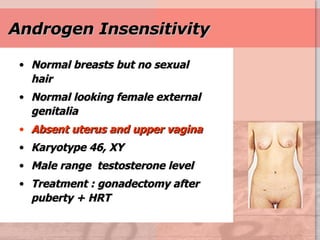
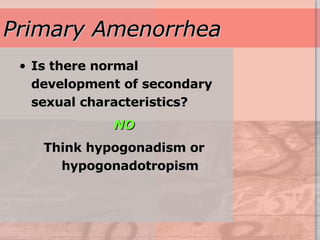
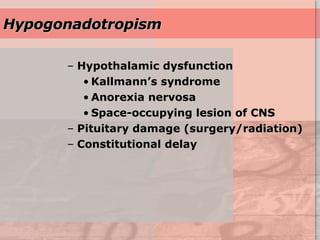
Amenorrhea is defined as the absence of menstruation. It can be primary, occurring before age 16, or secondary, occurring after menstruation has started. Possible causes of amenorrhea include issues with the hypothalamus, pituitary gland, ovaries, or uterus. Hypothalamic amenorrhea can be caused by stress, eating disorders, excessive exercise, or certain drugs. Evaluation of amenorrhea involves assessing sexual development, hormone levels, imaging tests, and response to medication challenges to determine the underlying cause. Treatment depends on the specific cause but may include hormone replacement, surgery, or lifestyle changes.