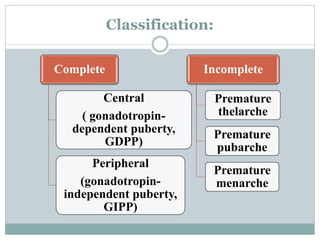
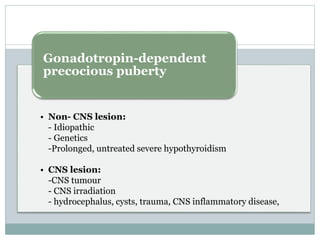
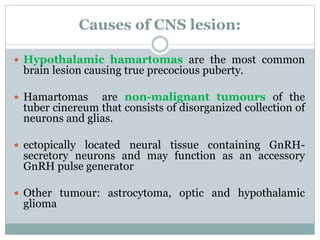
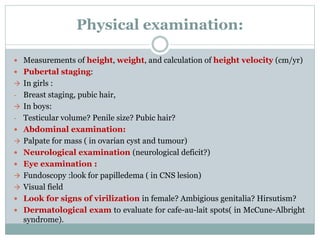
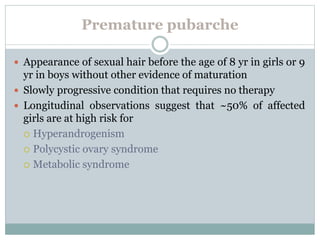
Precocious puberty is defined as the onset of secondary sexual characteristics before age 8 in girls and 9 in boys. It can be classified as central (gonadotropin-dependent) or peripheral (gonadotropin-independent) puberty. Central puberty is treated with GnRH agonists to slow progression, while peripheral causes like tumors require treatment of the underlying condition. Evaluation involves assessing pubertal development, growth, bone age, and hormone levels to distinguish central from peripheral puberty and identify any lesions.