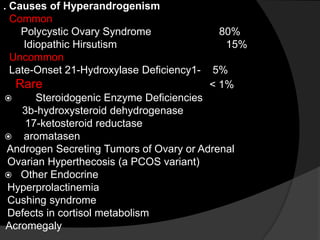
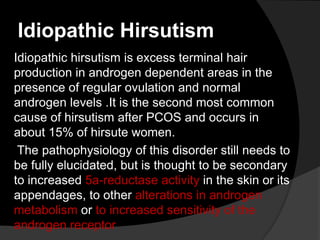
Secondary amenorrhea is the absence of menses for more than three cycles or six months in women who previously had menses. Pregnancy is the most common cause. The document outlines the step-by-step process for evaluating secondary amenorrhea, including ruling out pregnancy, assessing medical history, performing a physical exam, basic lab tests, and follow-up testing and evaluation if initial results require further investigation. Treatment options are provided for common causes like hyperprolactinemia, ovarian failure, hyperandrogenism, and Asherman's syndrome.