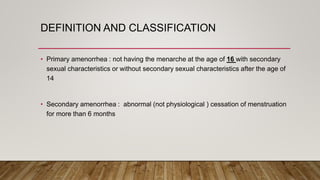
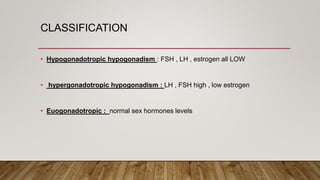
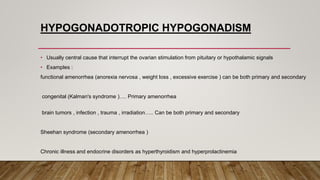
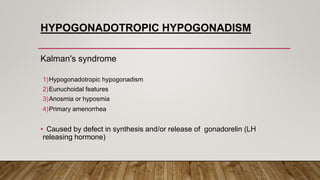
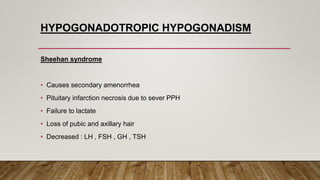
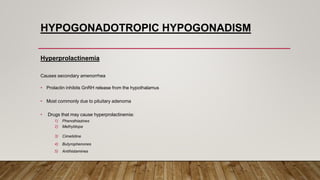
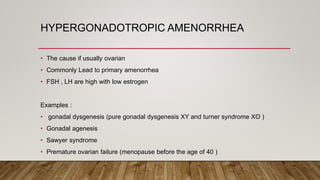
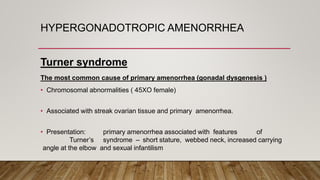
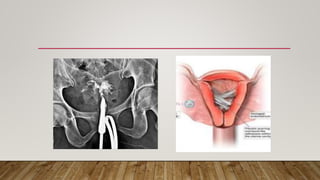
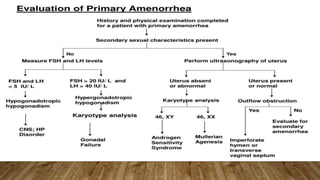
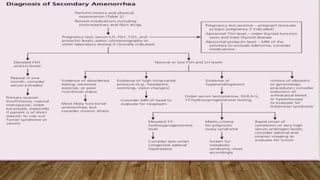
This document defines and classifies different types of amenorrhea, including primary and secondary amenorrhea. It discusses the main causes of amenorrhea, grouping them into hypogonadotropic hypogonadism (low FSH and LH), hypergonadotropic hypogonadism (high FSH and LH), and euogonadotropic amenorrhea (normal FSH and LH levels). Specific conditions that can cause each type are outlined, such as functional amenorrhea, Sheehan's syndrome, premature ovarian failure, and Mayer-Rokitansky-Küster-Hauser syndrome. The evaluation of a patient with amenorrhea is also briefly discussed.