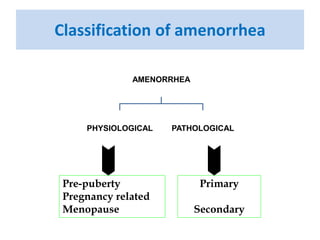
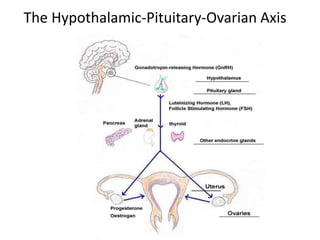
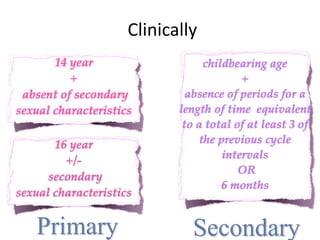
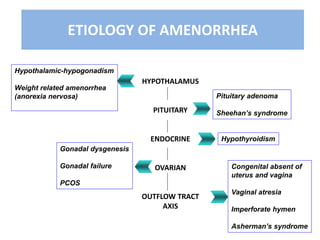
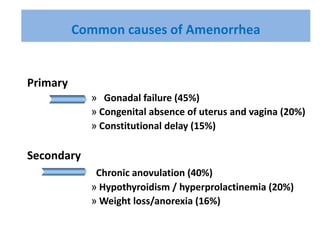
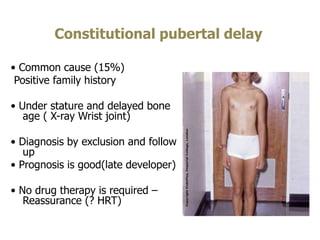
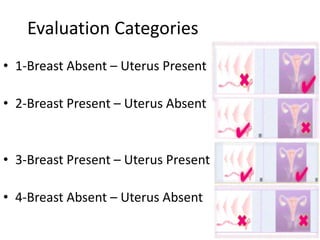
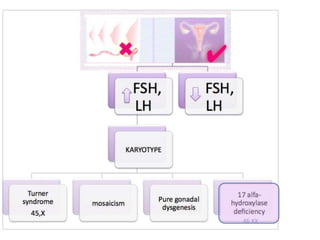
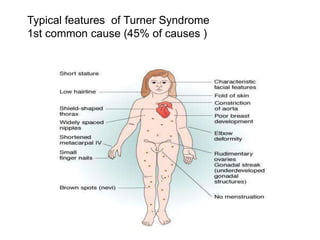
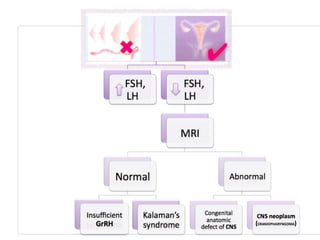
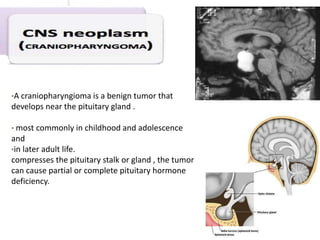
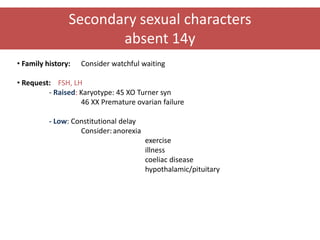
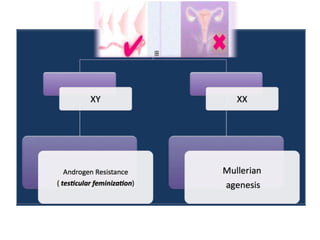
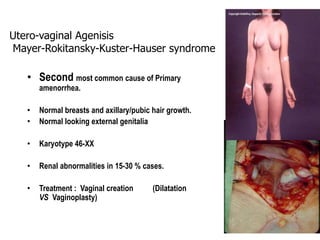
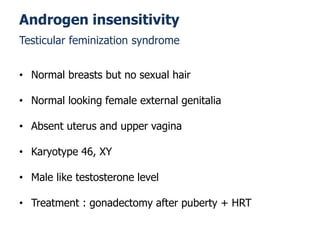
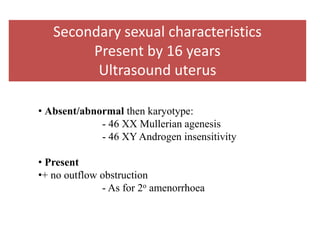
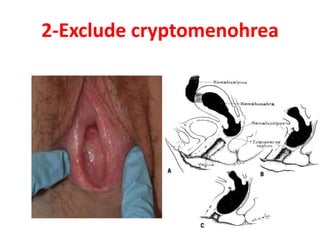
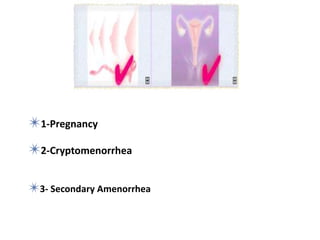
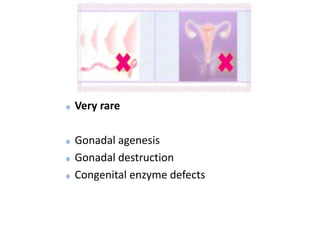
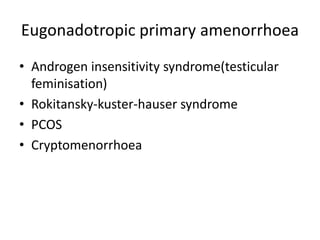
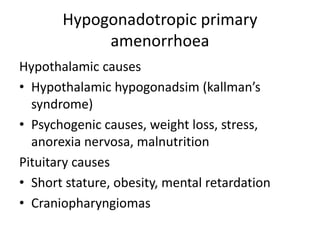
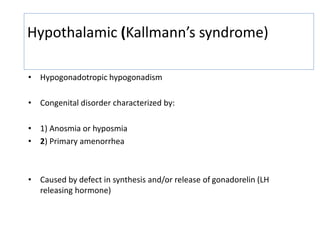
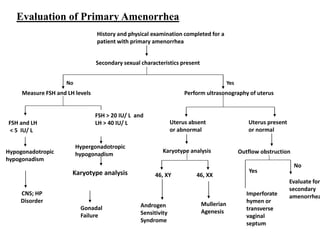
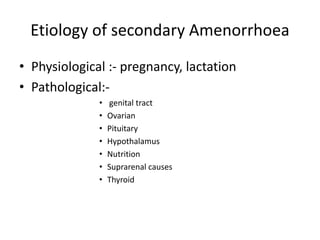
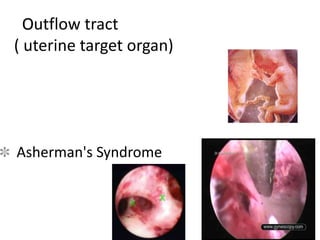
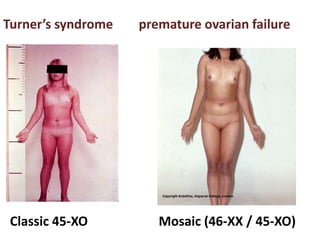
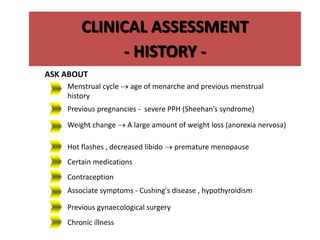
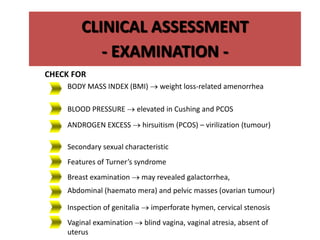
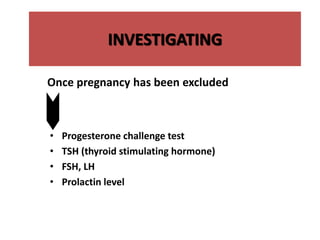
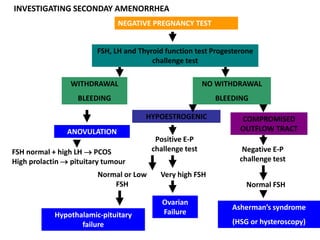
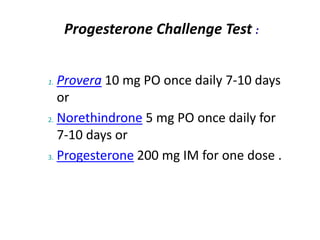
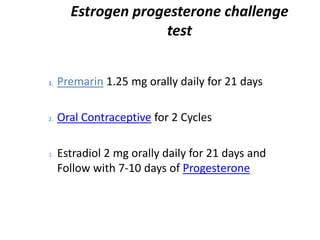
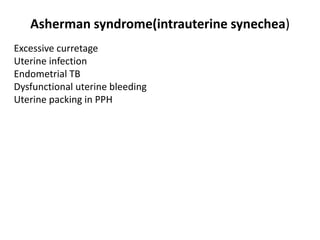
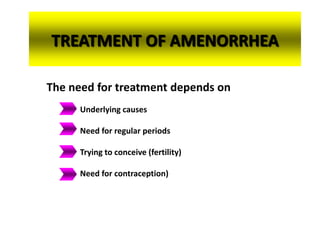
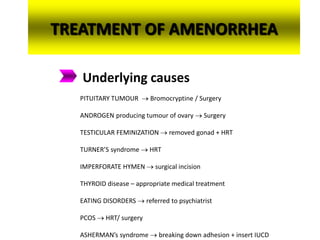
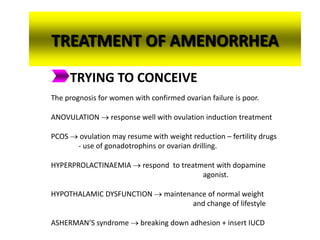
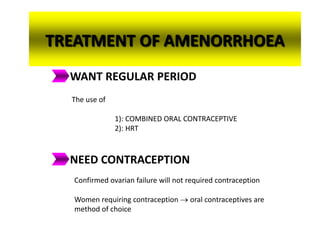
This document provides information on amenorrhea, including its classification and causes. It discusses the hypothalamic-pituitary-ovarian axis and the various etiologies of primary and secondary amenorrhea at each level of the axis. Common causes of primary amenorrhea include müllerian agenesis, androgen insensitivity syndrome, and Turner's syndrome. The most common cause of secondary amenorrhea is pregnancy, while other causes include polycystic ovarian syndrome, thyroid disorders, weight loss, and pituitary tumors. Evaluation involves history, exam, hormone levels, imaging, and challenge tests. Treatment depends on the underlying etiology and addressing irregular periods, fertility, or contraception needs.