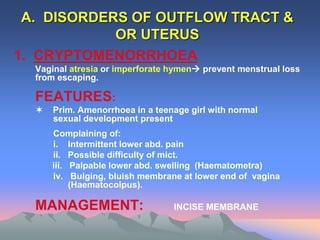
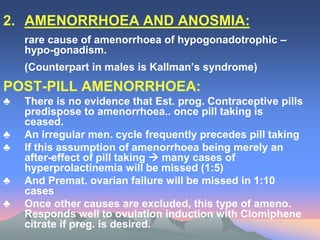
The document provides a comprehensive overview of primary and secondary amenorrhea, outlining their definitions, causes, and management strategies. Primary amenorrhea is characterized by the absence of menstruation by certain ages, while secondary amenorrhea is defined by a cessation of menstruation under specified conditions. The text discusses various etiologies, clinical approaches, diagnostic criteria, and specific types of amenorrhea, emphasizing the importance of thorough investigation and tailored treatment plans.