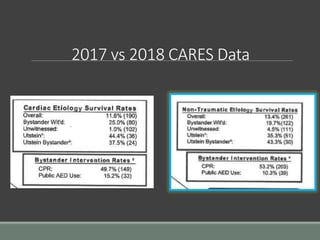
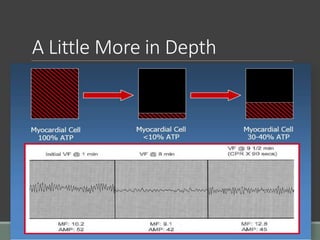
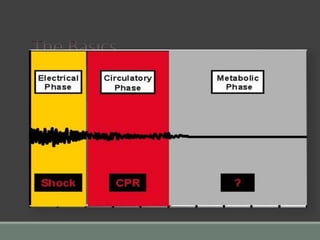
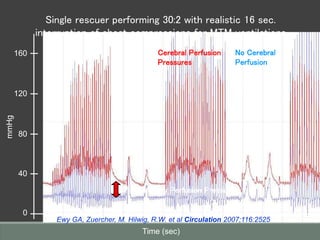
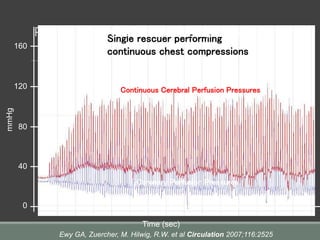
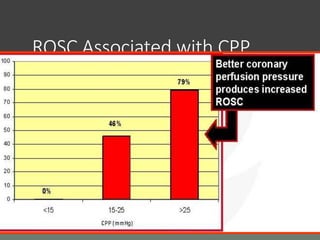
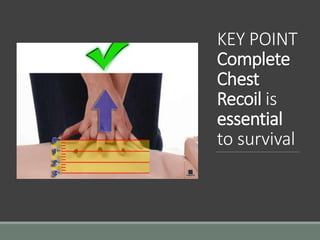
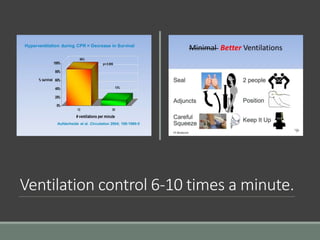
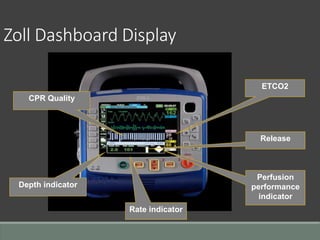
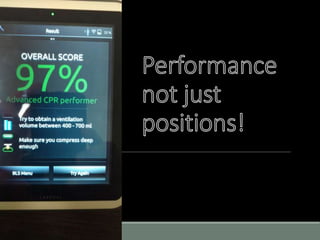
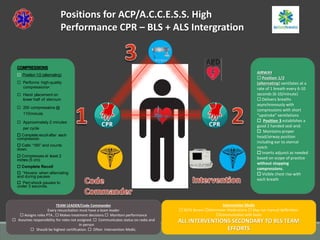
This document discusses high performance CPR techniques to improve outcomes for cardiac arrest patients. It provides 7 mantras of quality resuscitation and discusses key aspects of effective CPR including maintaining a rate of 100-120 compressions per minute, compressing at least 2 inches deep, fully releasing pressure between compressions, minimizing interruptions, and limiting ventilations to 6-10 per minute. The document outlines Ada County's model for high performance CPR using defined roles and positions to focus on continuous, high-quality chest compressions. It also reviews the science demonstrating improved perfusion and survival rates associated with minimizing interruptions and maintaining coronary and cerebral perfusion pressures.