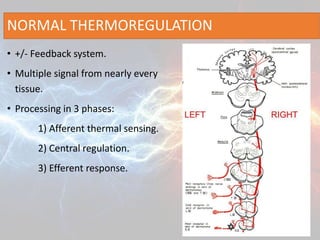
1. Humans tightly regulate their core body temperature around 37°C through feedback mechanisms involving thermal sensing receptors, central processing in the hypothalamus, and efferent responses like vasoconstriction and shivering.
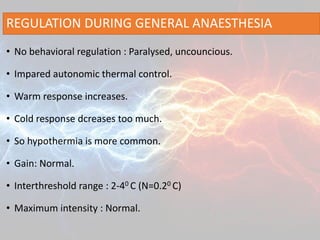
2. During general anesthesia, thermoregulation is impaired as behavioral responses are removed and autonomic responses like shivering and vasoconstriction are decreased. This commonly leads to unintended hypothermia from heat loss exceeding the body's ability to generate heat.
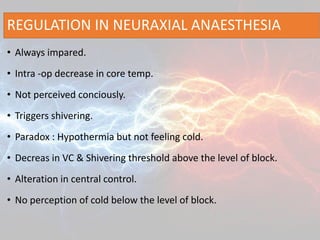
3. Regional anesthesia also impairs thermoregulation by blocking cutaneous vasoconstriction and decreasing the shivering threshold, potentially resulting in hypothermia if not monitored. Active warming and other