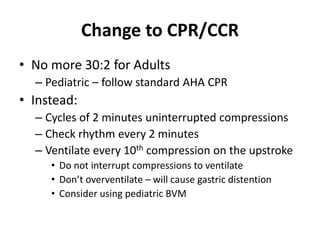
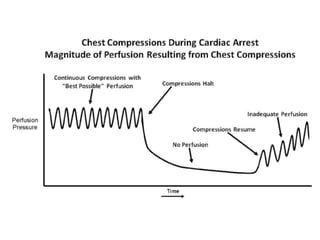
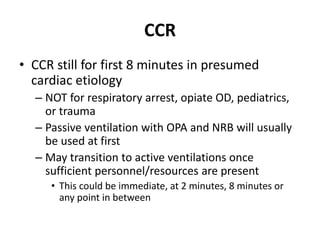
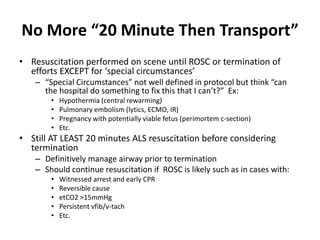
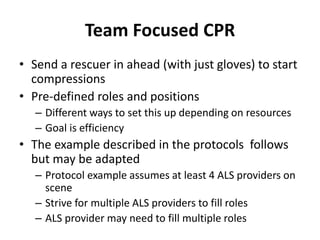
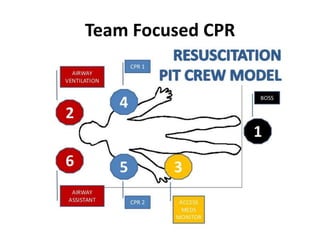
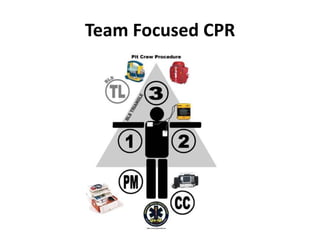
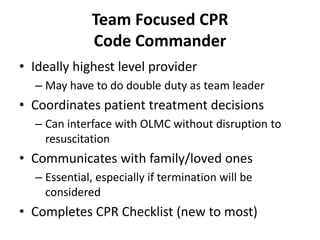
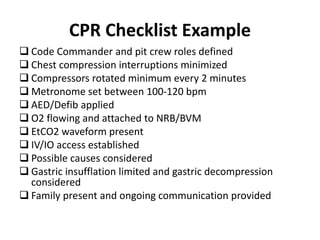
The 2016 CT state EMS protocol update emphasizes minimally interrupted, high-quality CPR. It changes adult CPR to continuous compressions for 2 minutes without pausing for breaths. For cardiac arrests, CCR is recommended for the first 8 minutes using passive ventilation before transitioning to active ventilations. Resuscitation should be performed on scene until ROSC or termination of efforts, except in special circumstances. The protocol introduces team-focused CPR with designated compressor, airway, and vascular roles to optimize efficiency. It also provides a CPR checklist for the code commander. Mechanical CPR may be considered in settings where high-quality manual CPR is difficult.
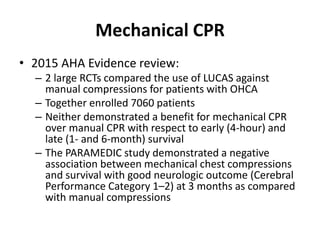
![Mechanical CPR
• 2015 AHA Recommendation:
– “The evidence does not demonstrate a benefit with the use of
mechanical piston devices for chest compressions versus manual
chest compressions in patients with cardiac arrest.”
– “Mechanical piston devices may be considered in specific
settings where the delivery of high-quality manual compressions
may be challenging or dangerous provided that rescuers strictly
limit interruptions in CPR during deployment and removal of the
devices.” Ex:
• Limited rescuers available
• Prolonged CPR
• During hypothermic cardiac arrest
• In a moving ambulance
• In the angiography suite
• During preparation for extracorporeal CPR [ECPR]),](https://image.slidesharecdn.com/20161006cprccrupdate-161008144038/85/2016-10-06-cpr-ccr-update-18-320.jpg)