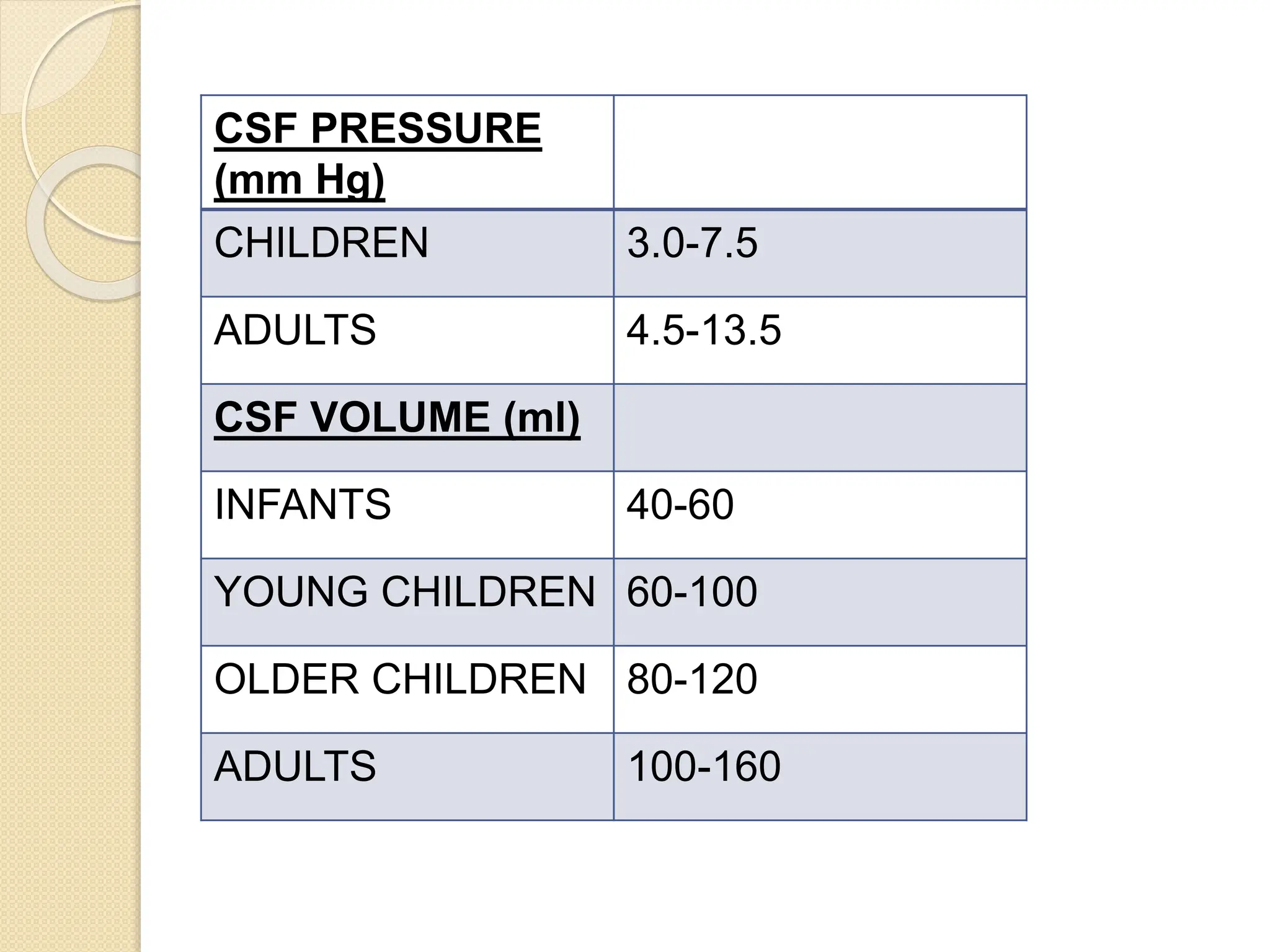
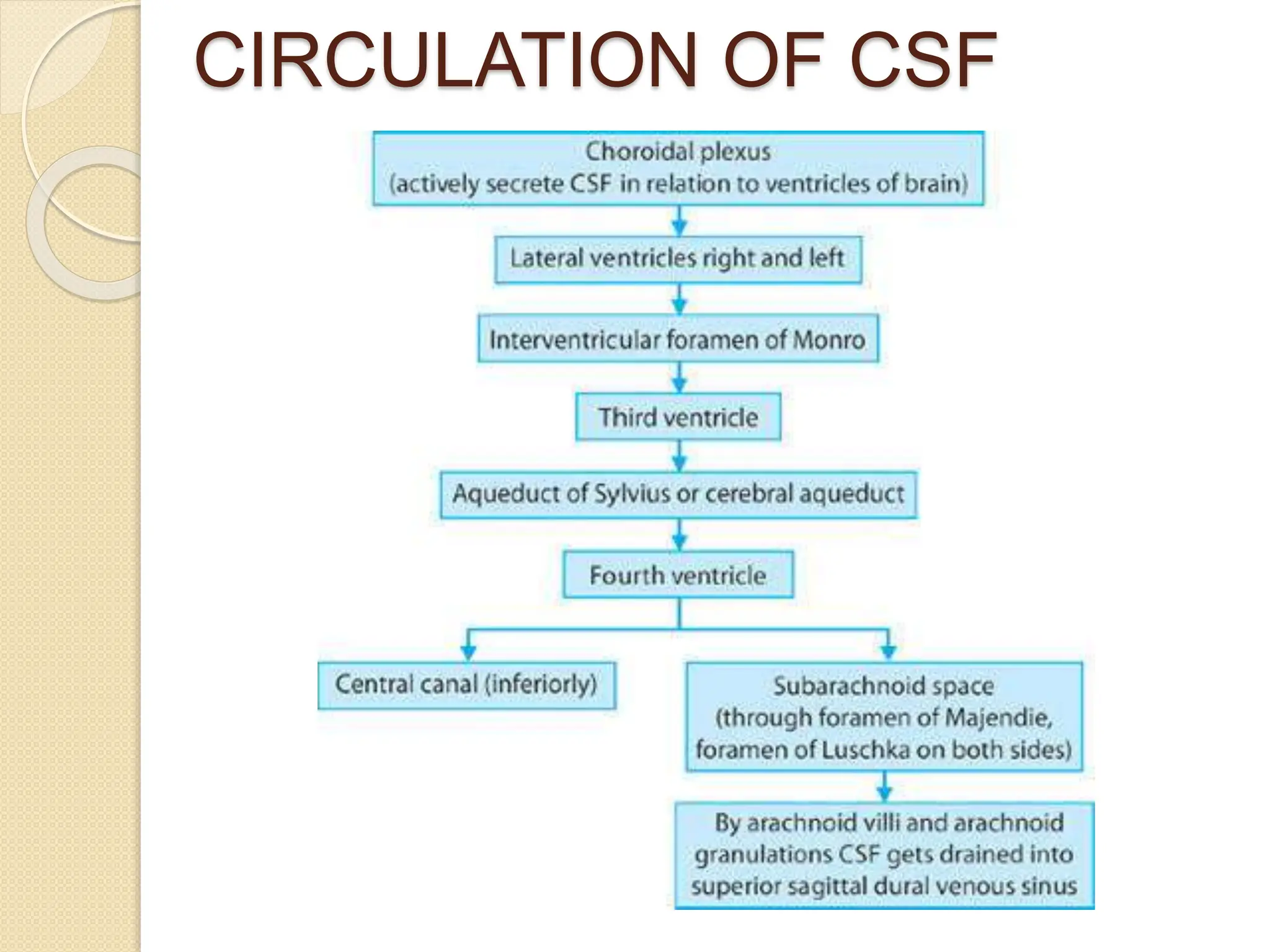
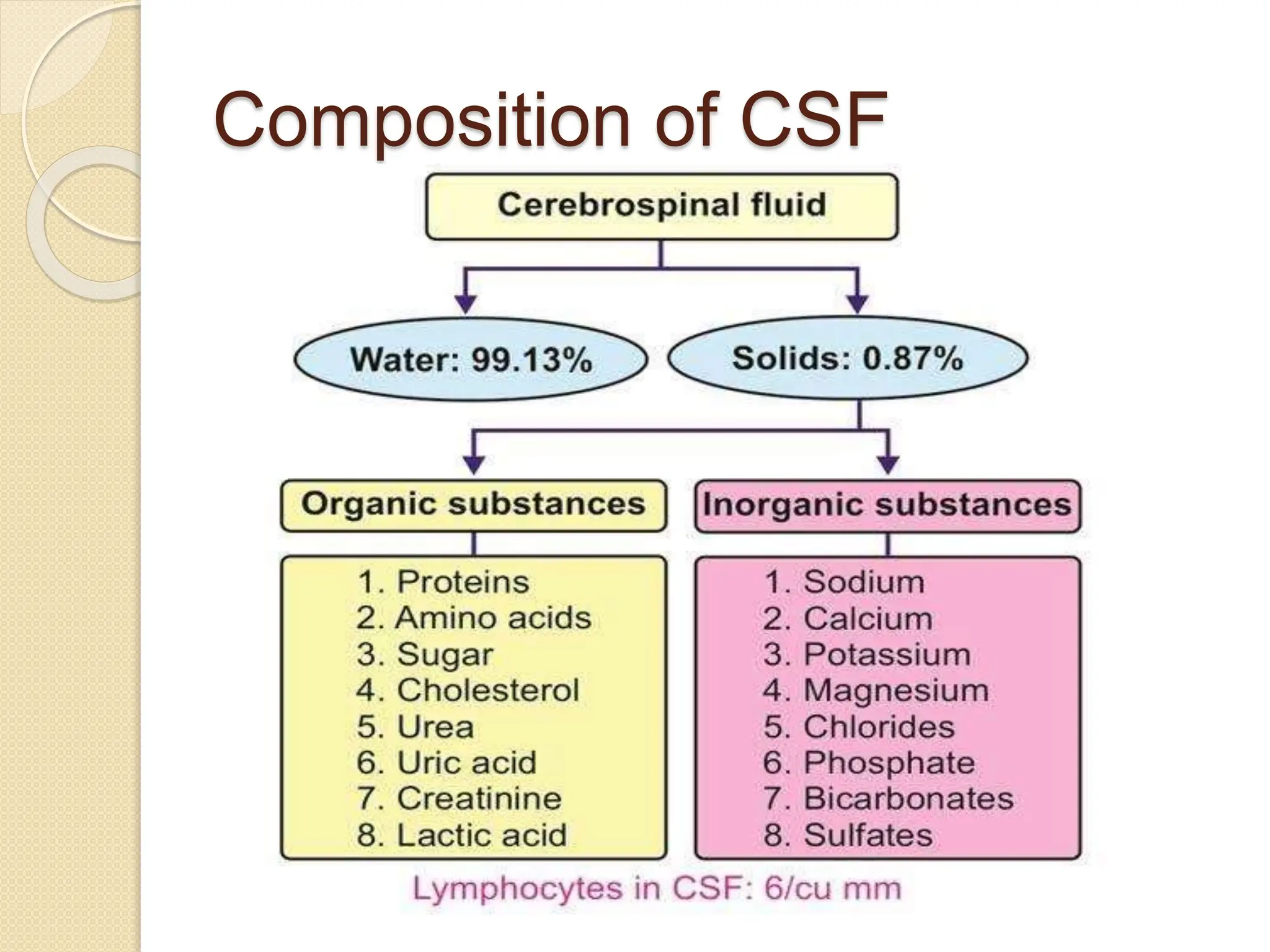
The document discusses cerebrospinal fluid (CSF) physiology, circulation, and its role in protecting the brain, providing nutrients, and removing waste. It details the formation and composition of CSF, factors affecting its production, and the regulation of intracranial pressure, along with methods for measurement and treatment of conditions like hydrocephalus. Anesthesia management considerations in patients with increased ICP are also outlined, emphasizing careful monitoring and specific drug protocols.