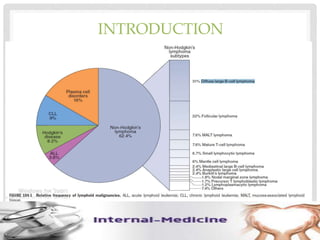
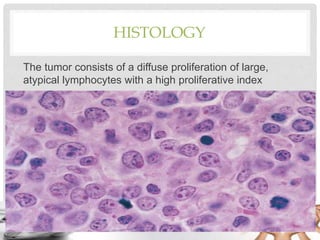
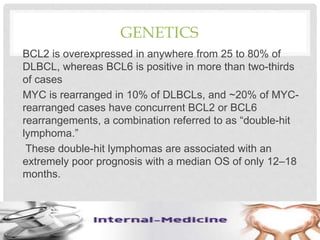
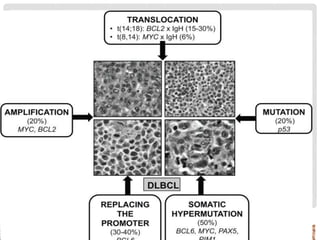
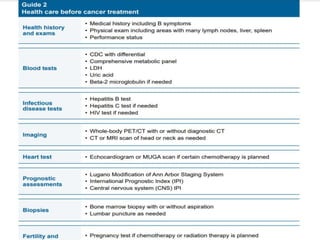
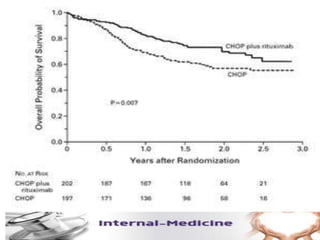
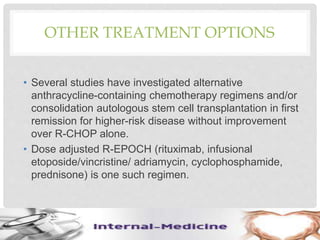
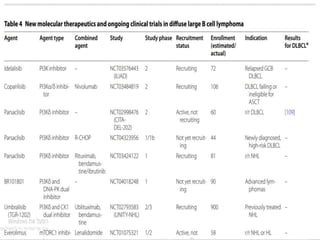
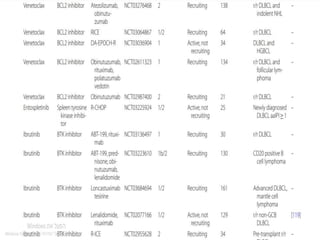
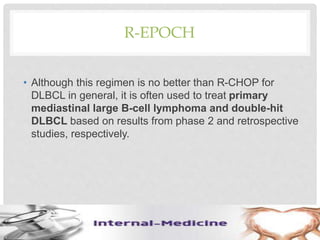
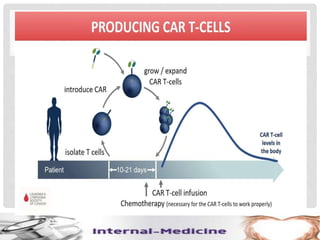
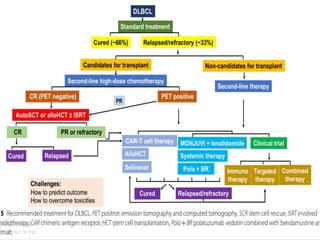
This document provides an overview of diffuse large B-cell lymphoma (DLBCL), including epidemiology, risk factors, presentation, histology, genetics, therapy, and treatment options. DLBCL is the most common subtype of non-Hodgkin lymphoma. The standard first-line treatment is rituximab combined with cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). For early stage disease, options include full chemotherapy or abbreviated chemotherapy with radiation. Advanced disease is treated with full chemotherapy. Refractory cases may be treated with newer agents or CAR T-cell therapy.