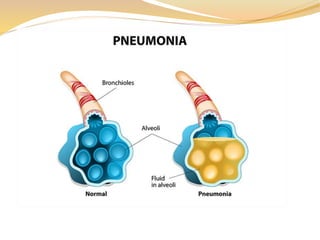
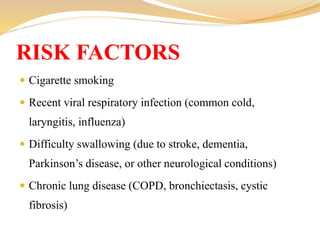
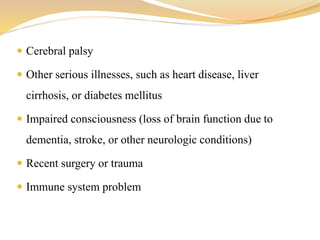
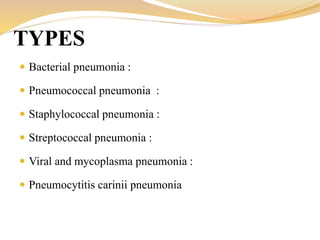
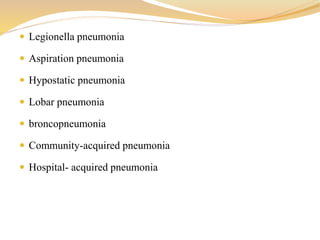
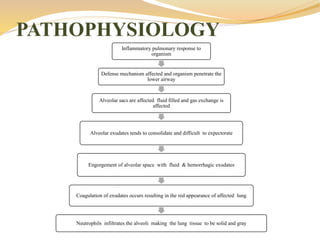
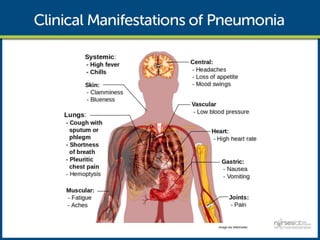
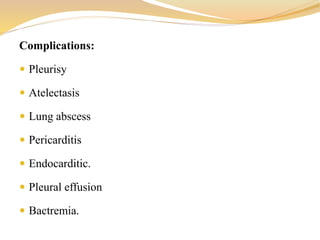
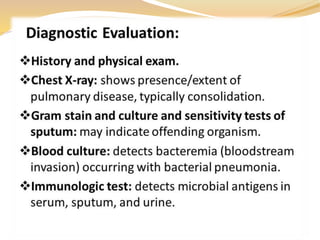
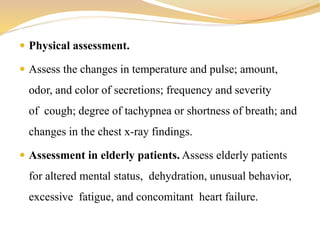
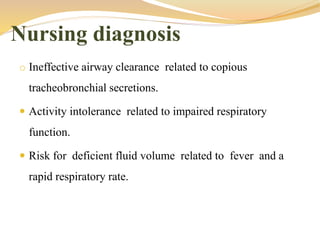
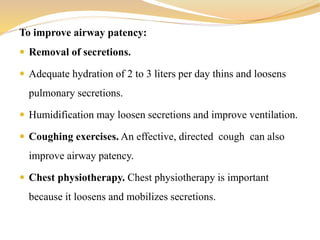
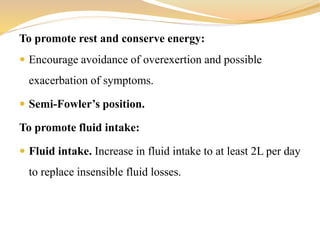
Pneumonia is an infection of the lungs that causes inflammation in the air sacs, making it difficult to breathe. It can be caused by bacteria, viruses, or fungi. The document discusses the causes, types, symptoms, complications, treatment including antibiotics and respiratory support, and nursing management of pneumonia with a focus on improving breathing, rest, hydration, and nutrition.