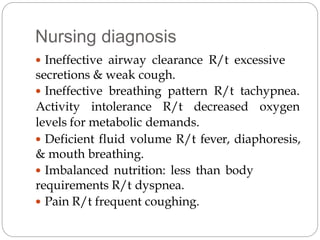
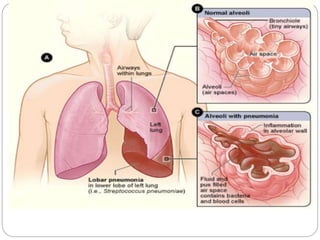
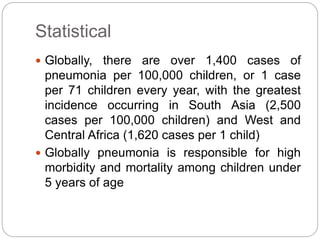
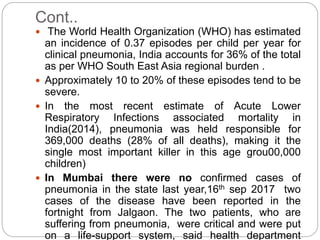
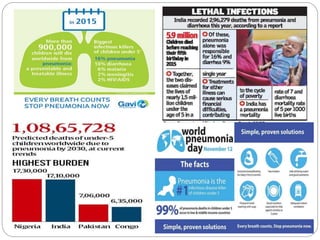
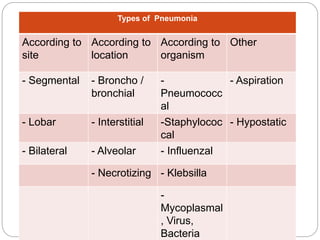
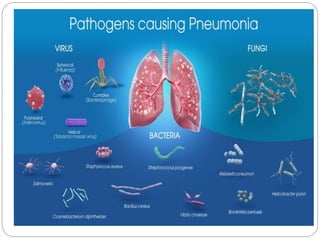
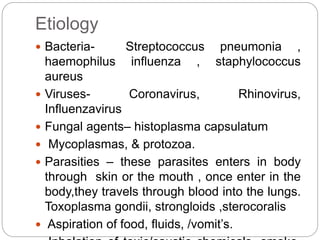
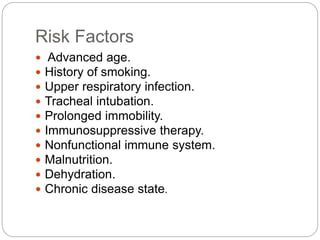
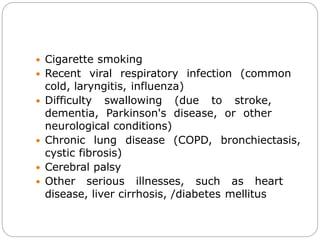
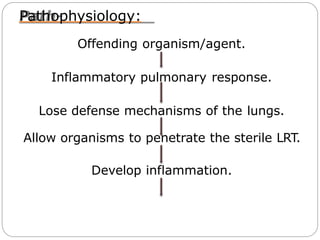
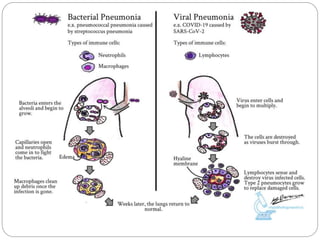
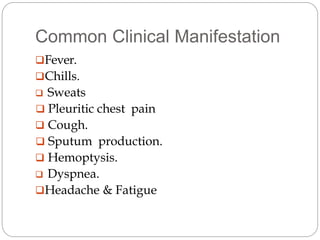
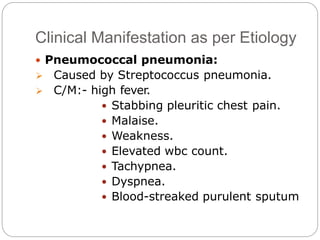
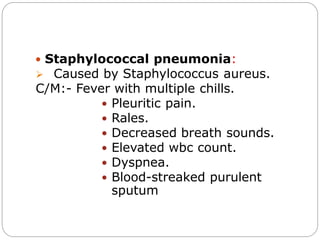
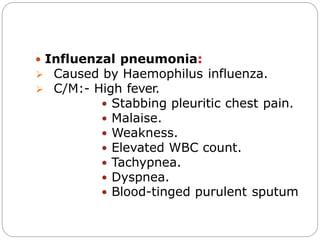
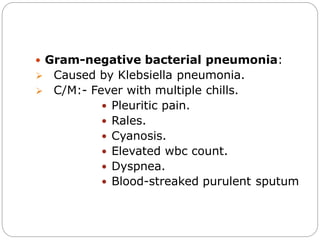
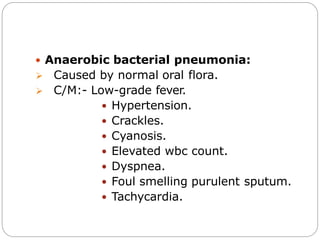
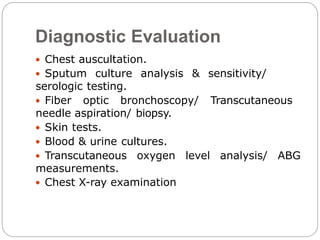
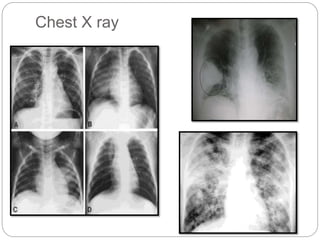
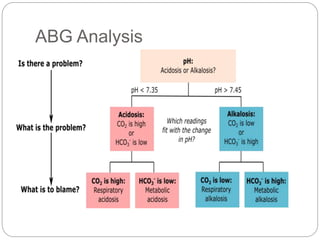
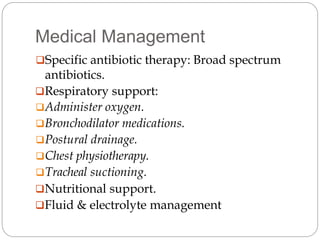
The document discusses pneumonia, defining it as an inflammatory process in the lung parenchyma that can lead to serious health issues, particularly in children under five years old, with high incidence rates in areas like South Asia and Africa. It covers various types, causes, risk factors, clinical manifestations, diagnostic evaluations, and management strategies for pneumonia. The document emphasizes the importance of medical and nursing management, patient education, and preventive measures to combat pneumonia effectively.
![Health Education
Instruct patient to continue taking antibiotics until
complete
Advice patient to increase activites graduallyafter
fever subsides
Advice patient that fatigue and weakness may
linger on]
Encourage breathing exercise
Instruct the patient to avoid fatigue , sudden
changes in temperature and excessive alcohol,
which lower resistance of pneumonia
Recommend influenza vaccine and pneumovax
to all pateints at risk .](https://image.slidesharecdn.com/pneumonia-201205072517/85/Pneumonia-32-320.jpg)