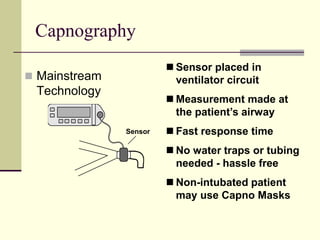
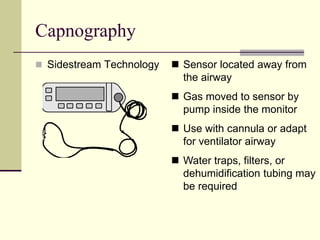
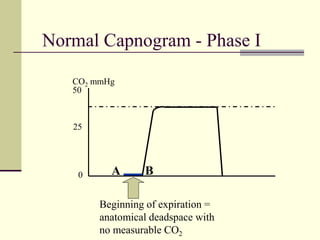
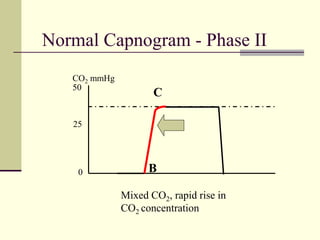
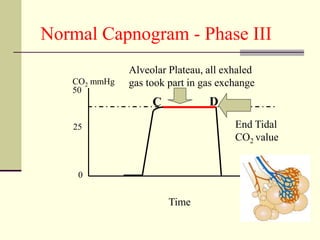
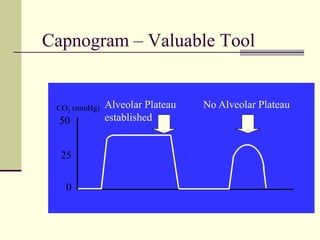
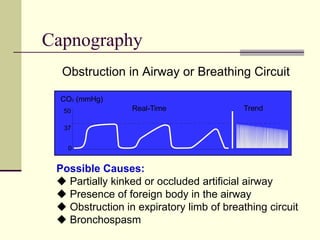
(1) Capnography depicts respiration by measuring exhaled carbon dioxide levels and the CO2 waveform; (2) The CO2 waveform can help validate ETCO2 values, assess airway integrity, and detect proper endotracheal tube placement; (3) Abnormal capnography readings can indicate issues like hypoventilation, hyperventilation, or airway obstruction and help guide clinical intervention.