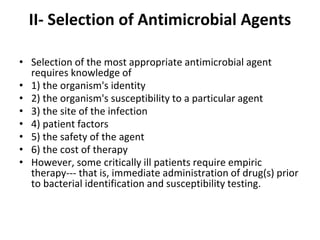
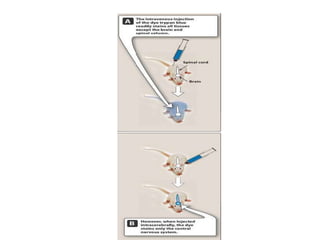
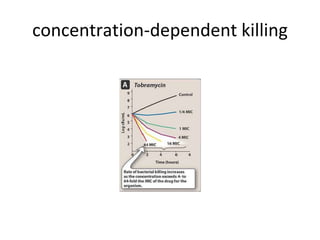
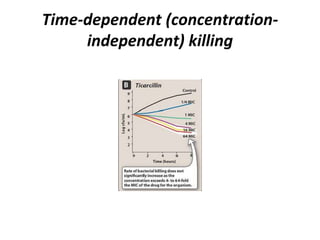
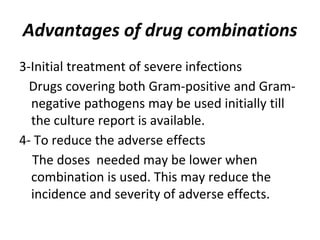
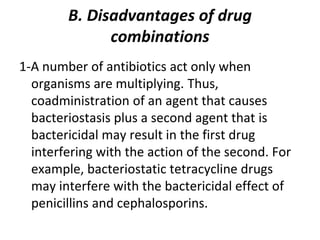
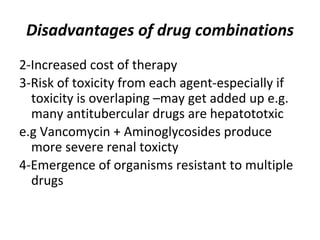
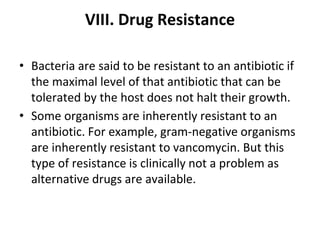
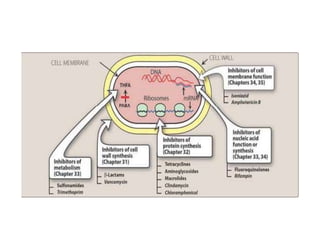
This document discusses principles of antimicrobial therapy. It covers selecting appropriate antimicrobial agents based on the infecting organism, site of infection, and patient factors. Empiric therapy may be needed before identification. Antimicrobial susceptibility testing guides treatment. Combination therapy has advantages like synergism but also disadvantages like increased resistance. Routes of administration and rational dosing are also discussed.