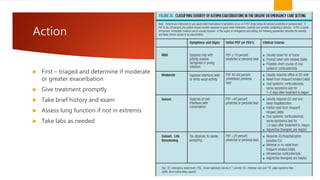
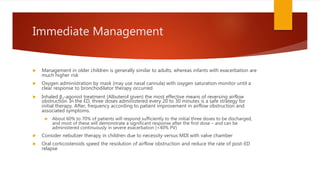
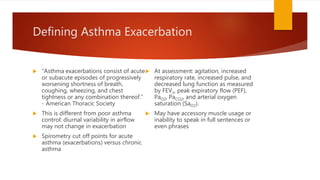
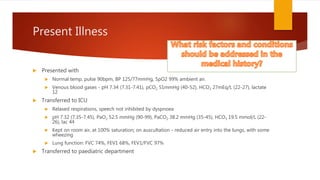
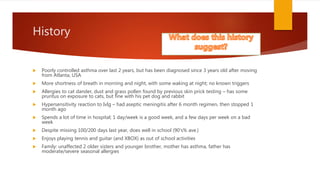
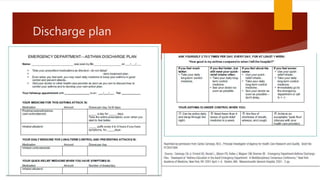
A 13-year-old male with a history of poorly controlled asthma presented to the pediatric ER with difficulty breathing and dry cough due to an exacerbation. His management included bronchodilator therapy, oxygen support, and assessment of lung function, along with an ICU transfer for severe symptoms. Discharge planning emphasized education on asthma management, realization of symptoms, and follow-up care.