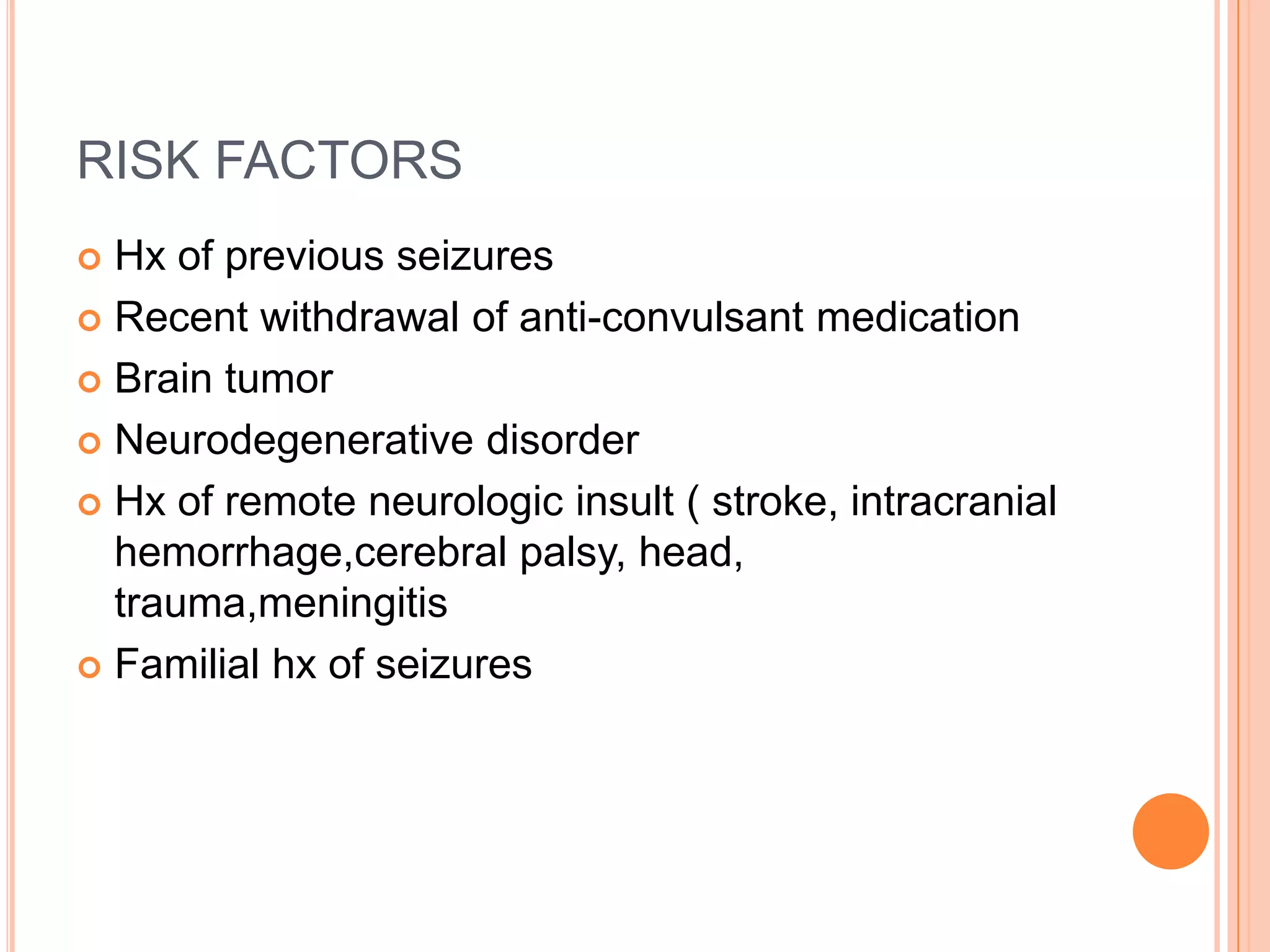
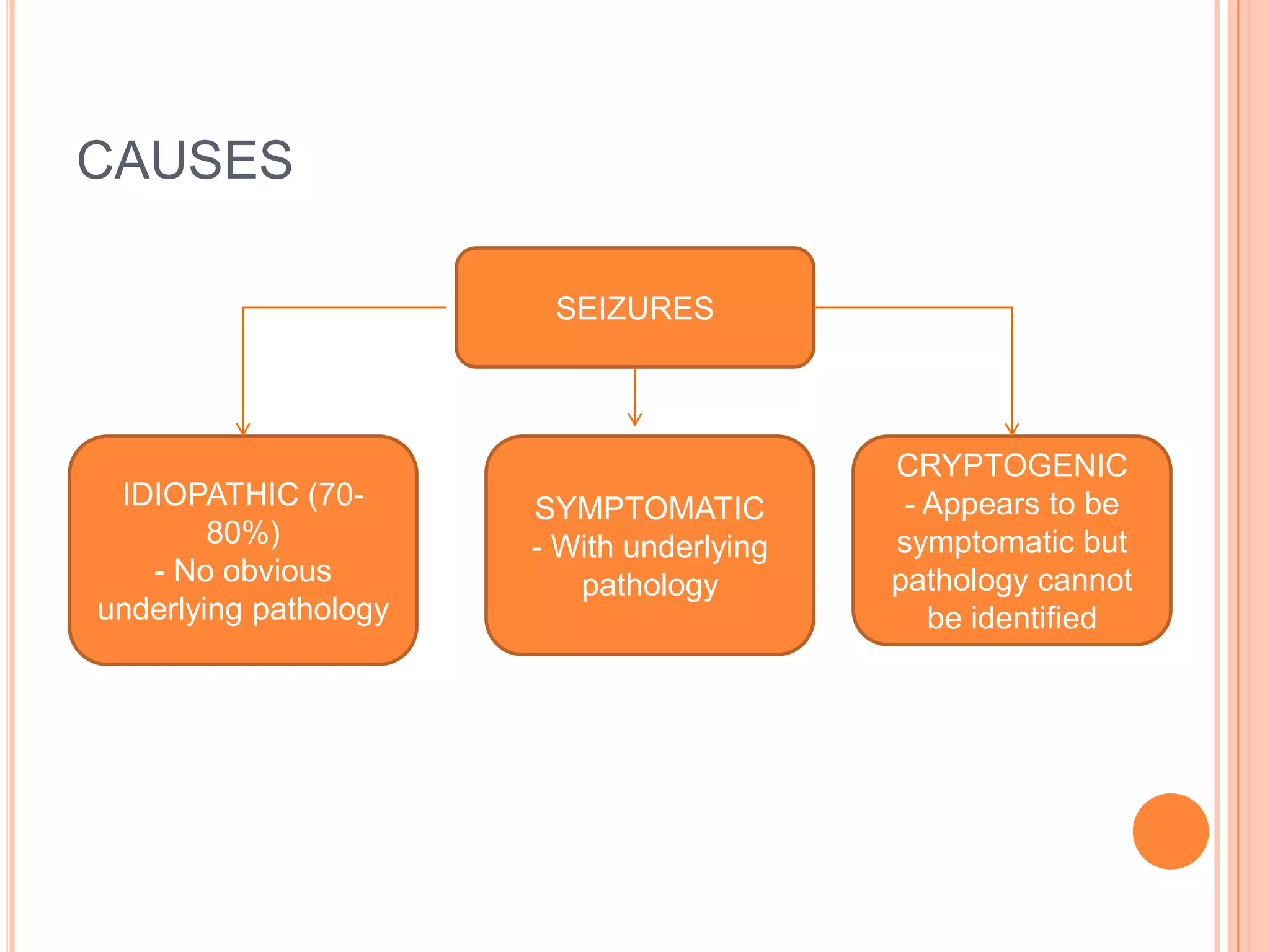
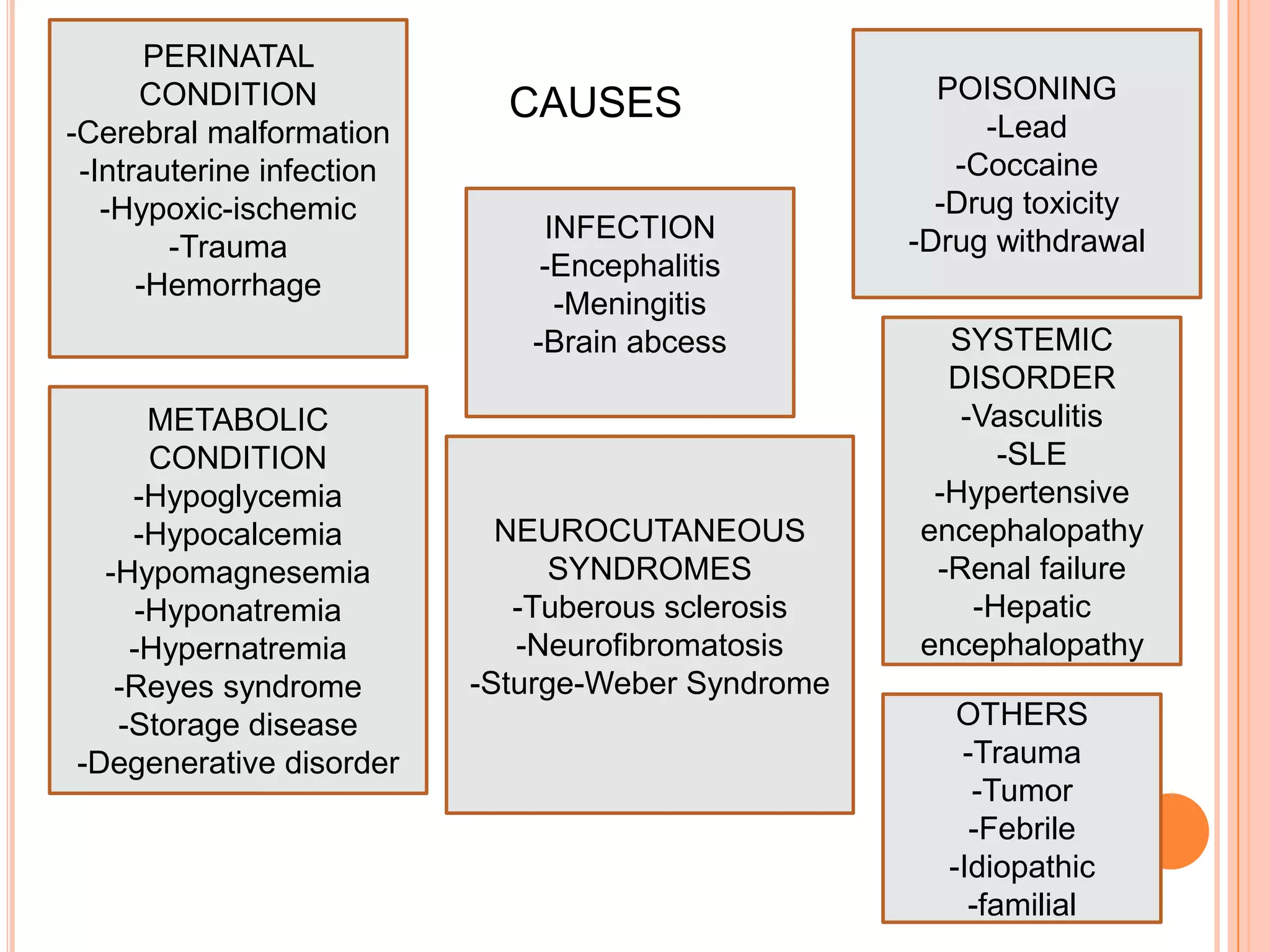
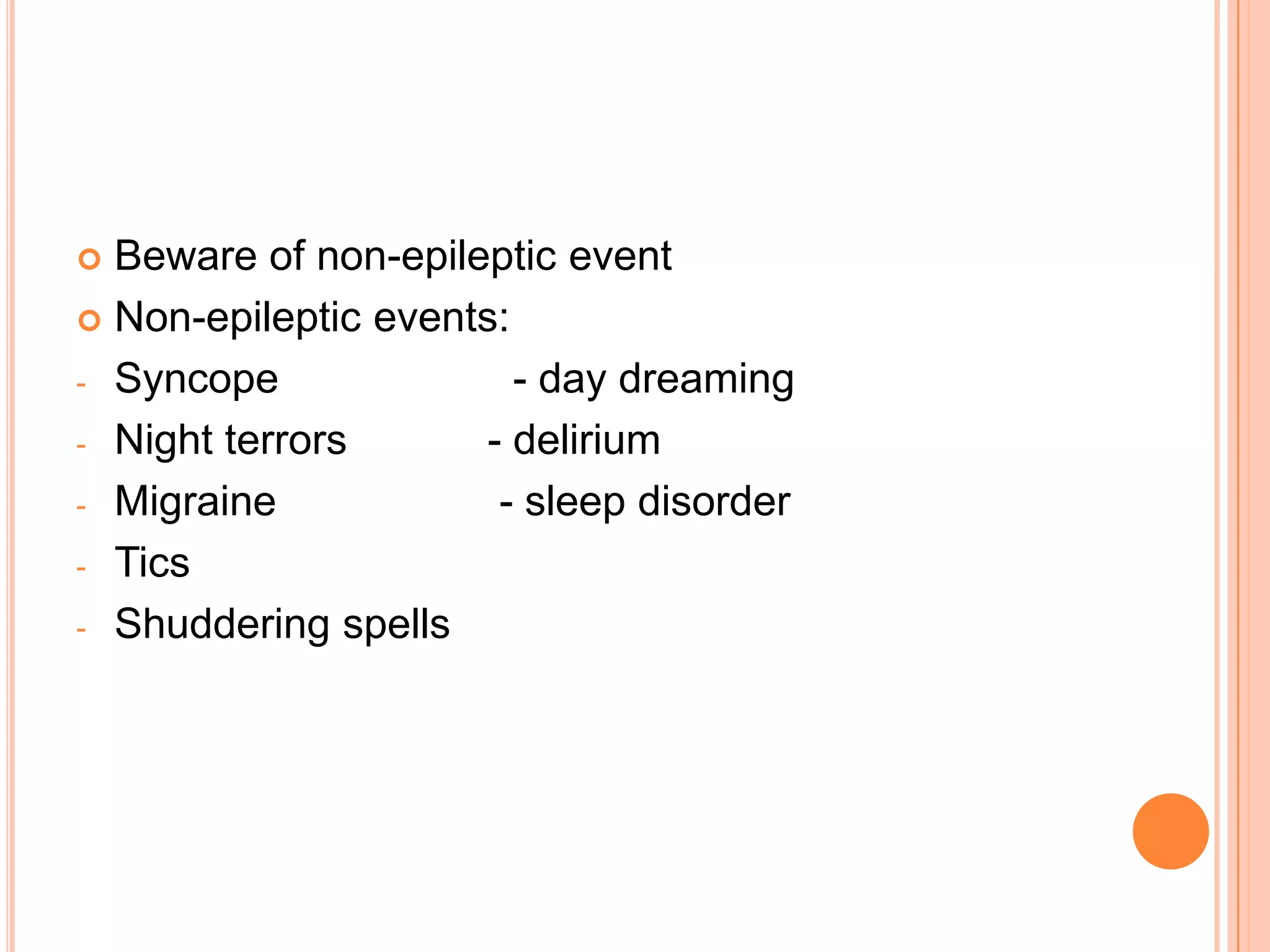
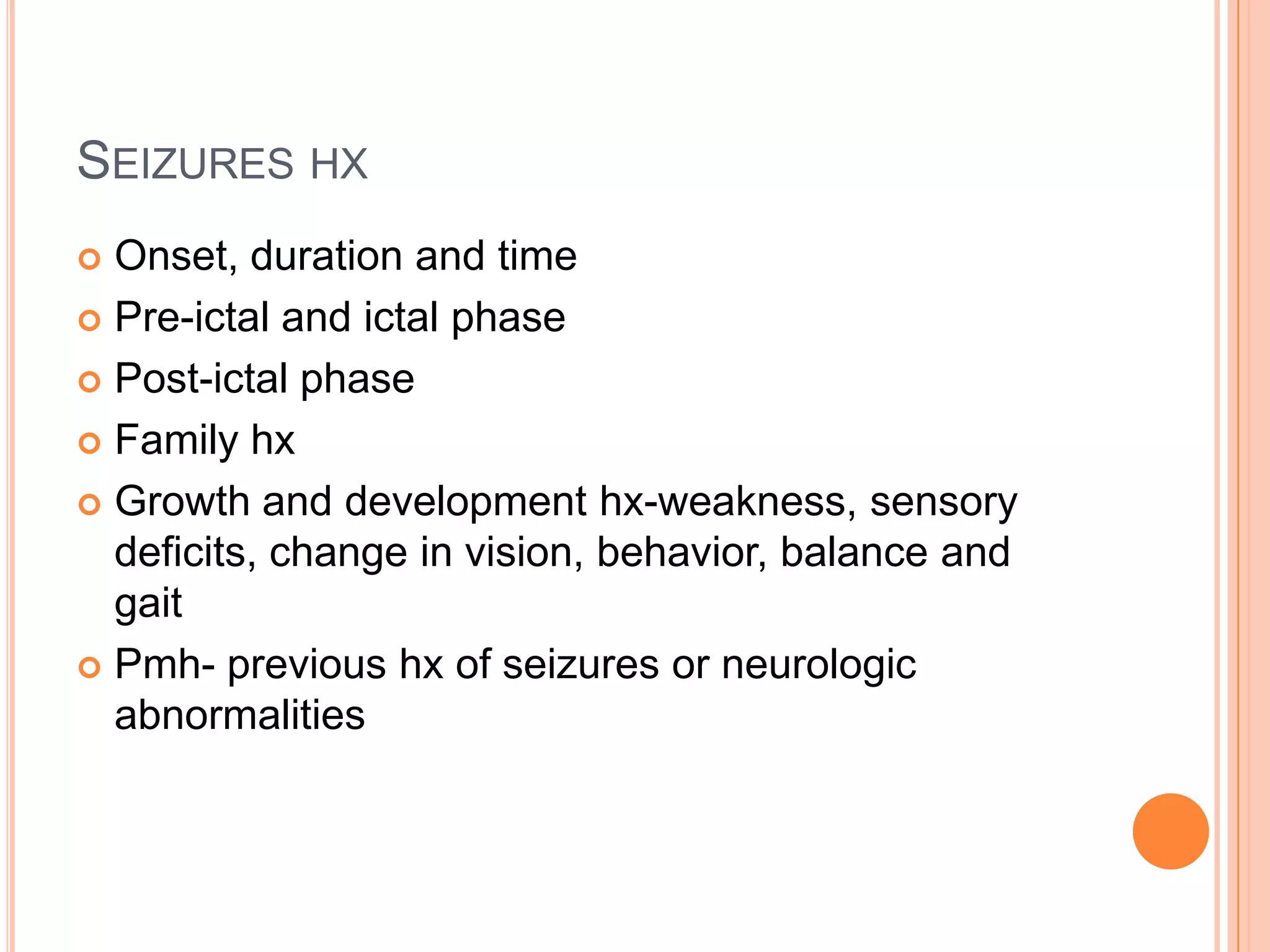
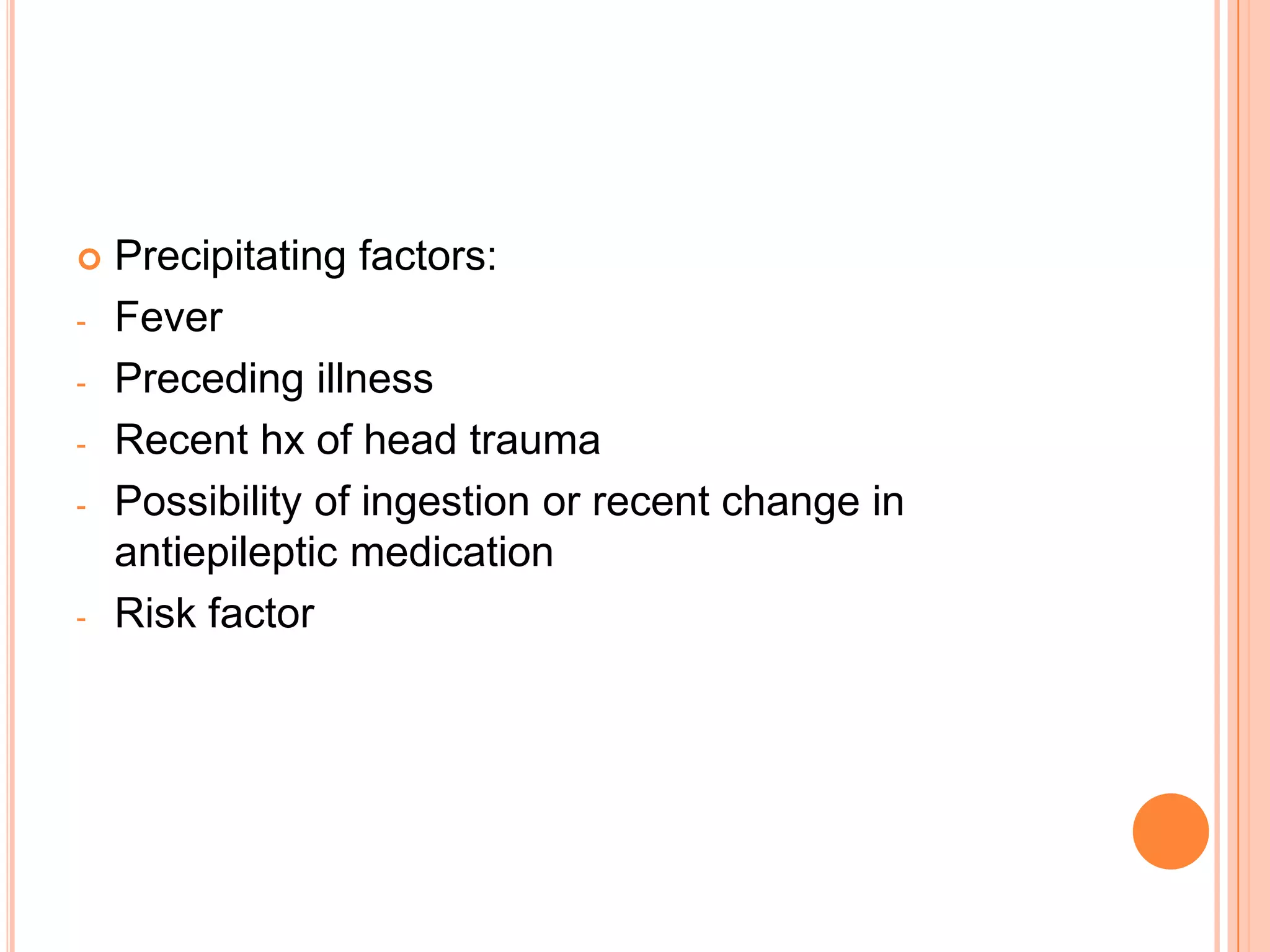
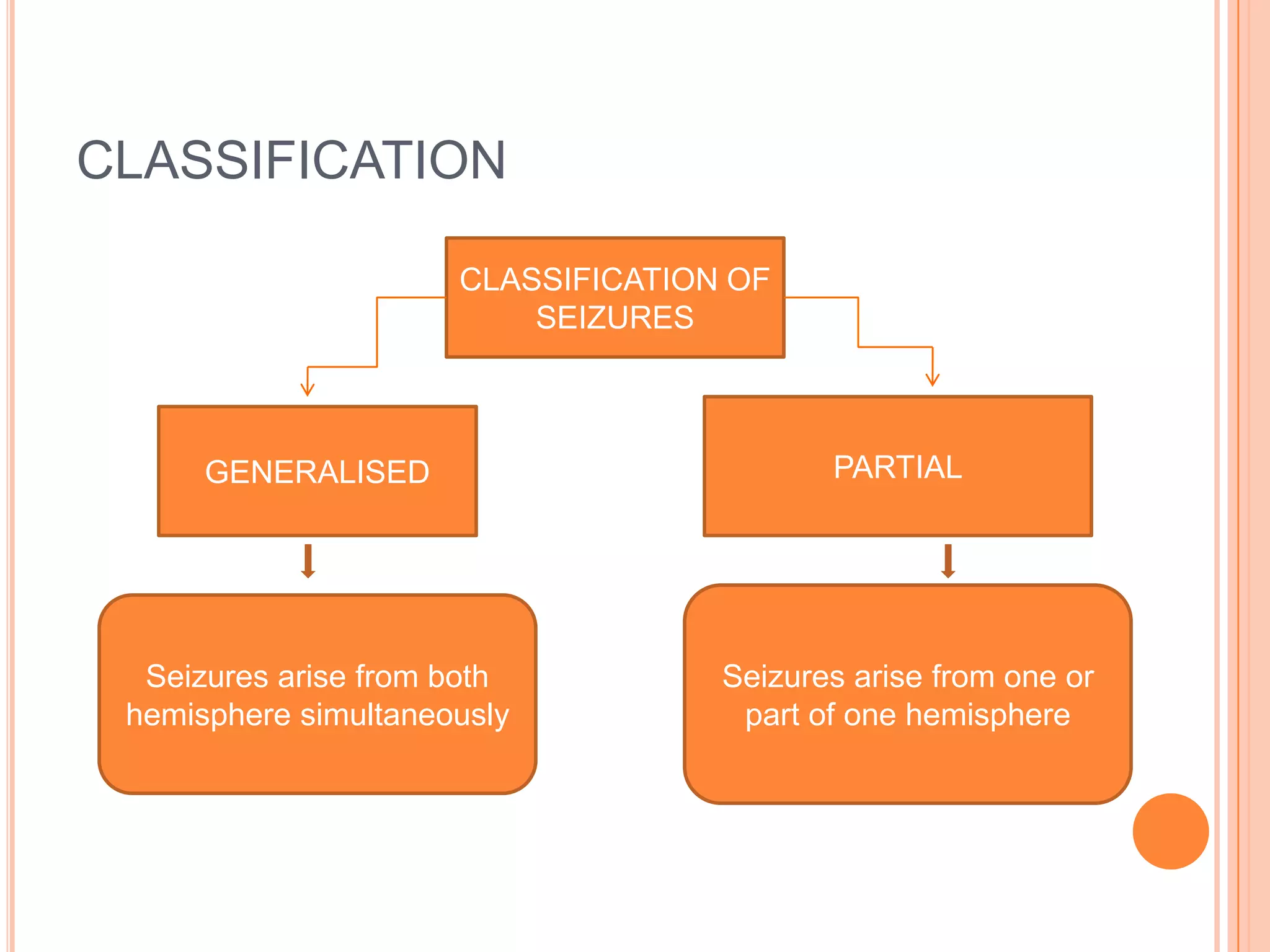
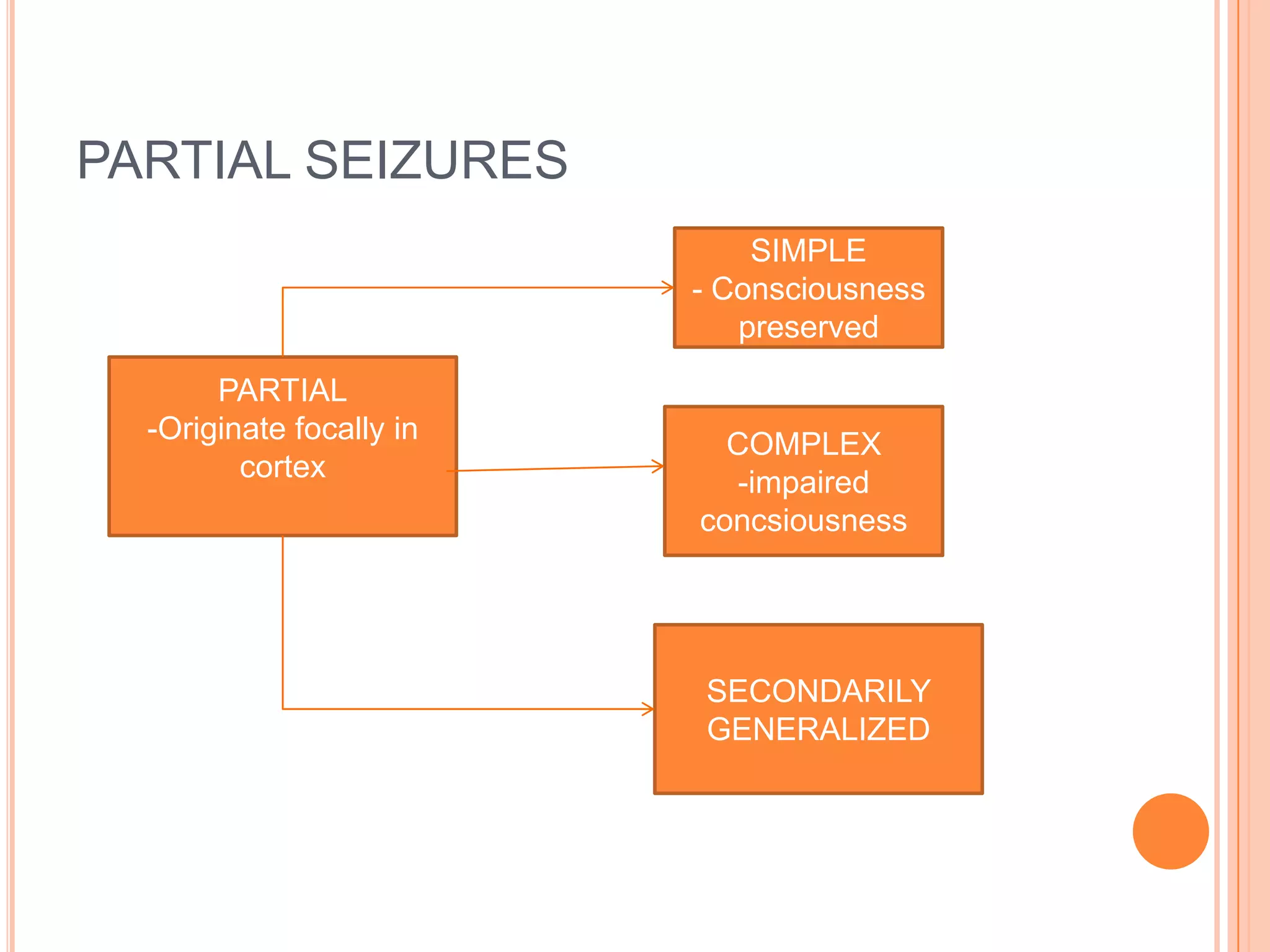
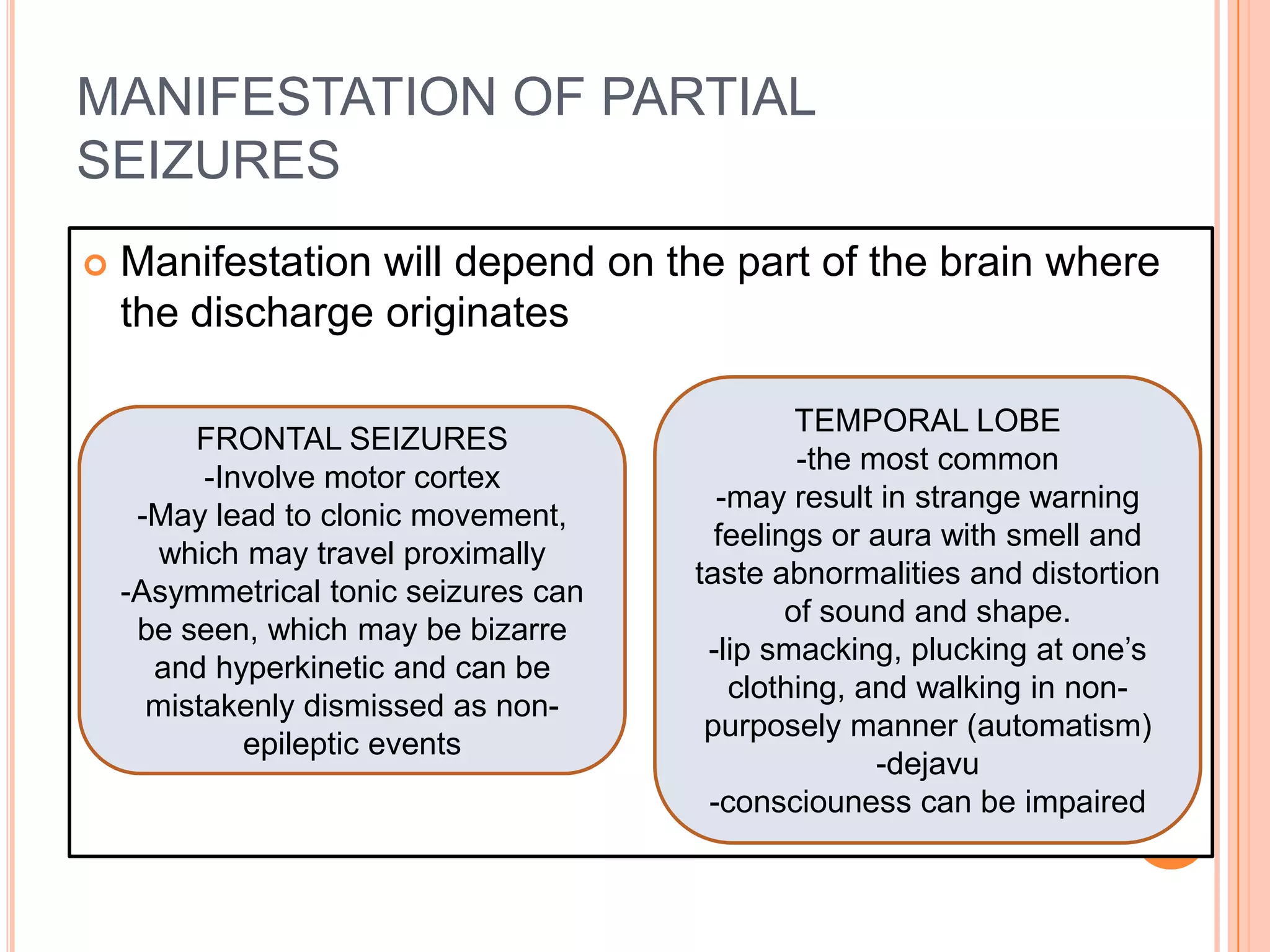
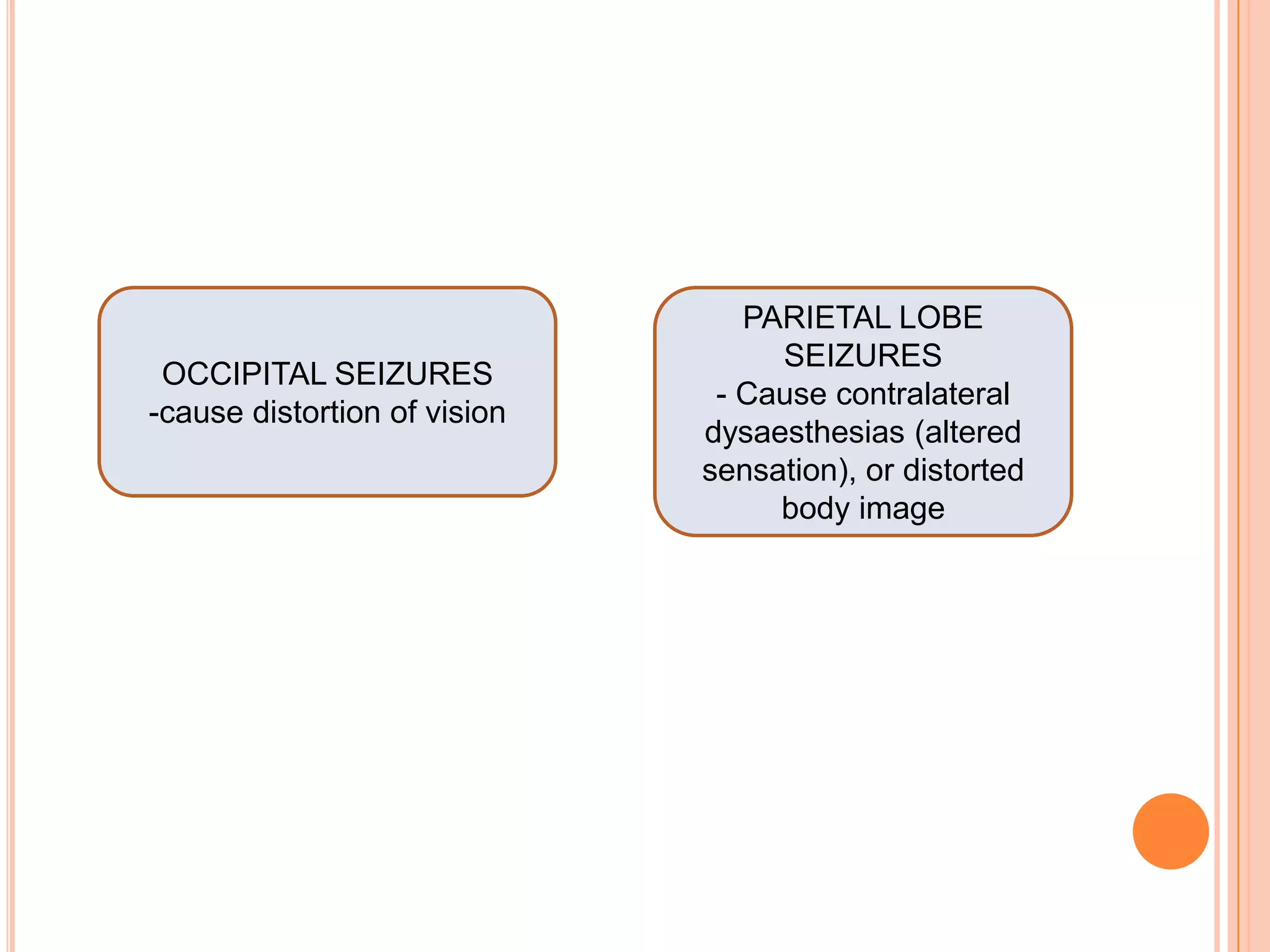
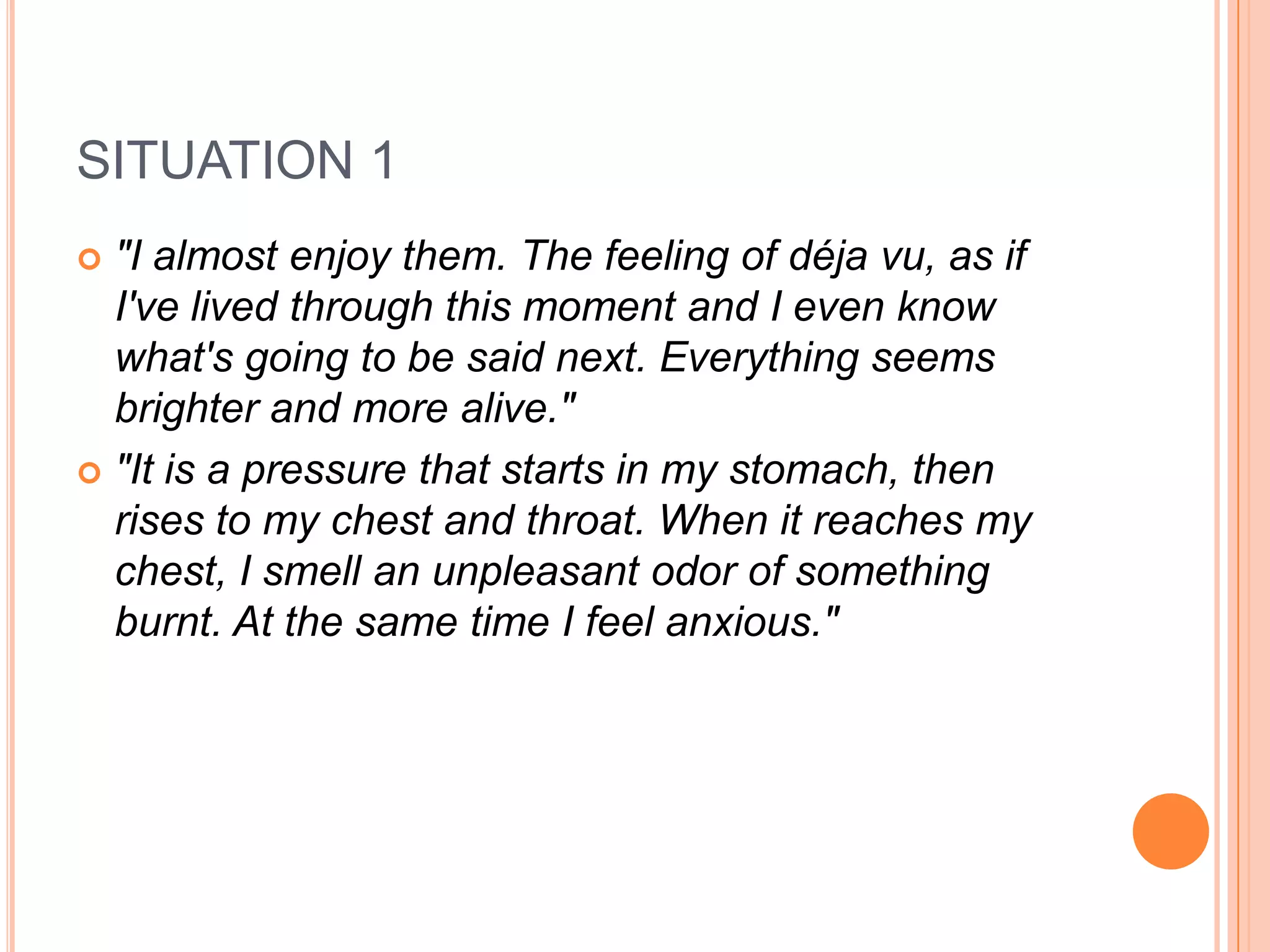
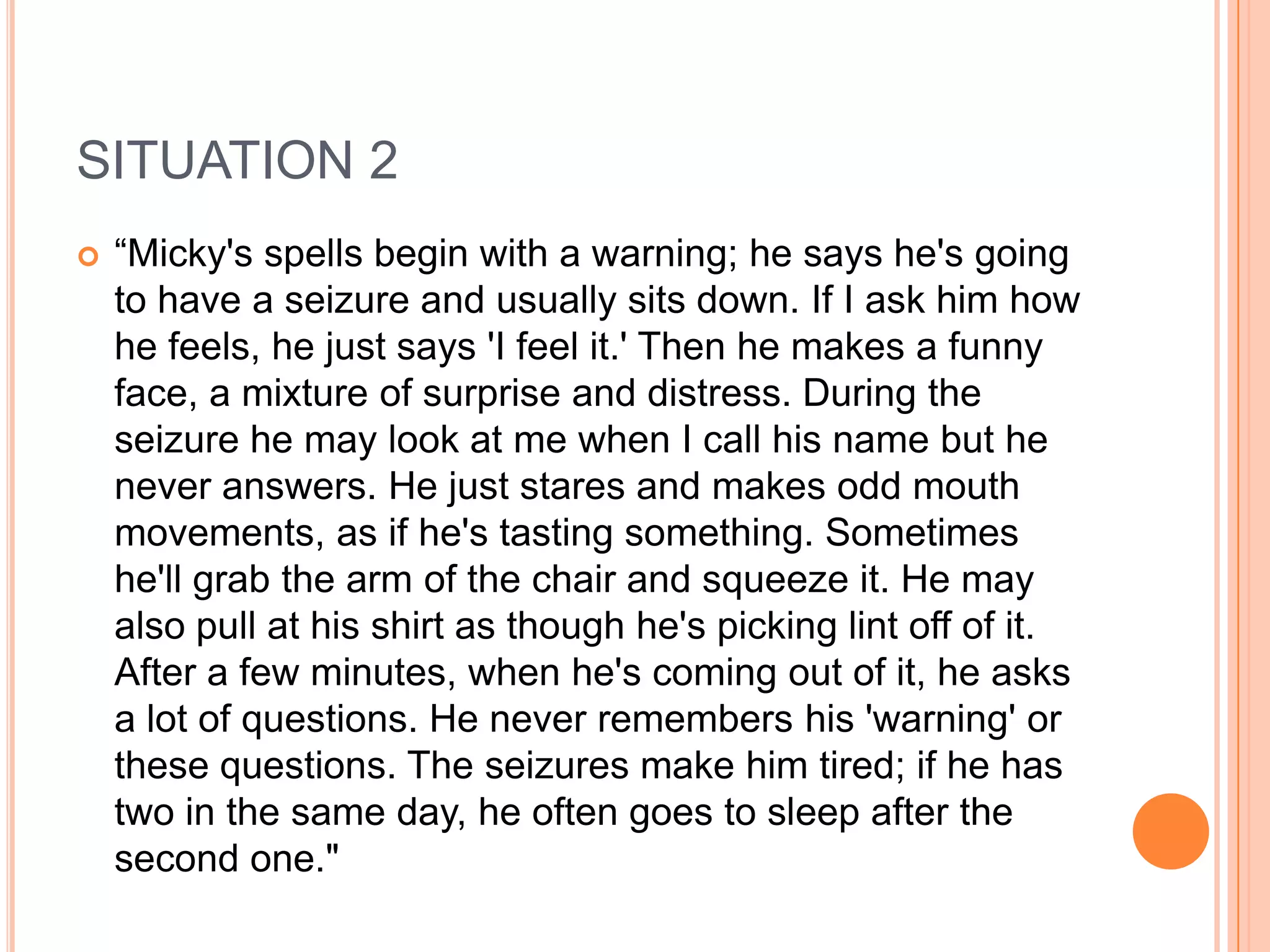
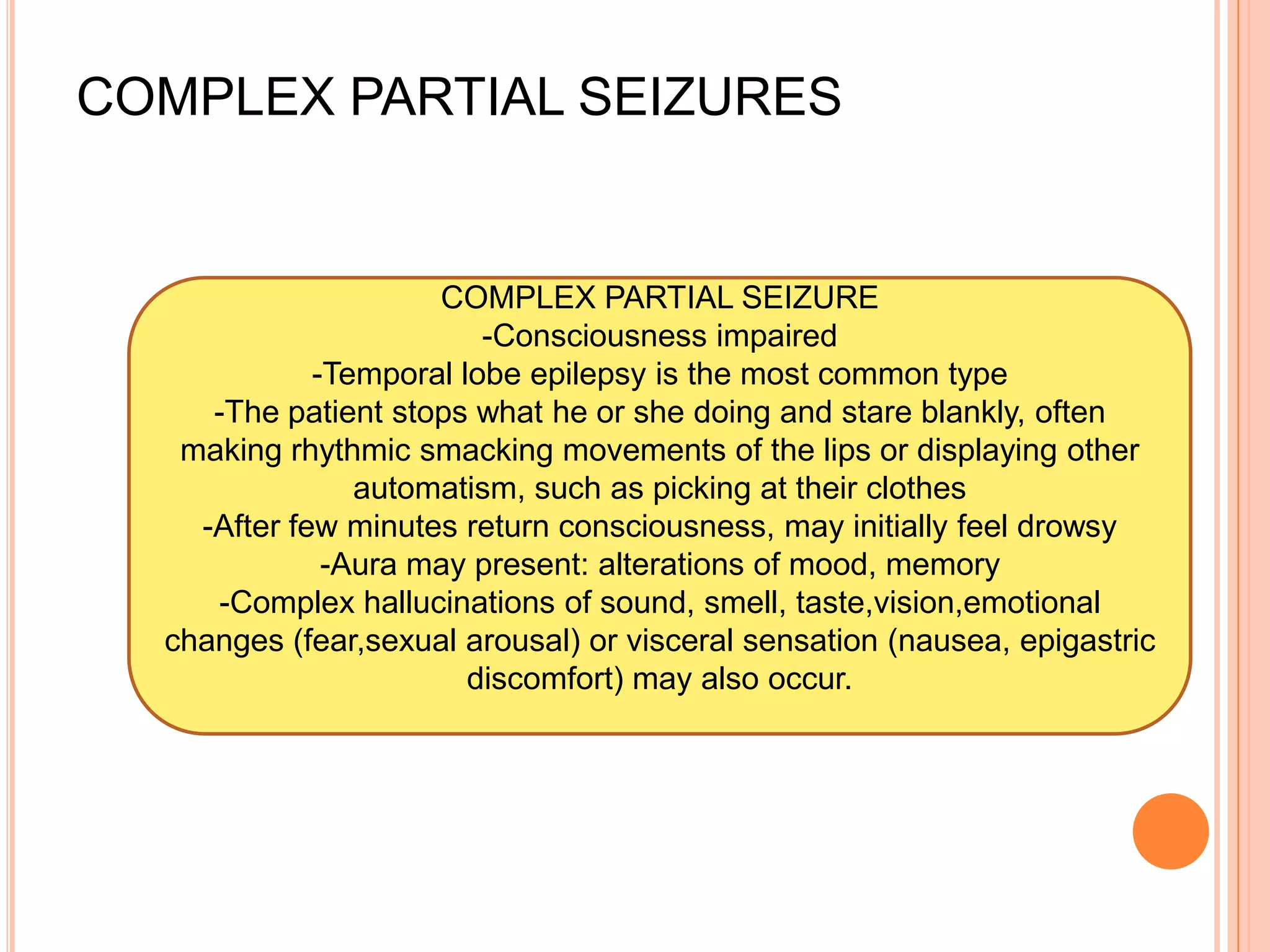
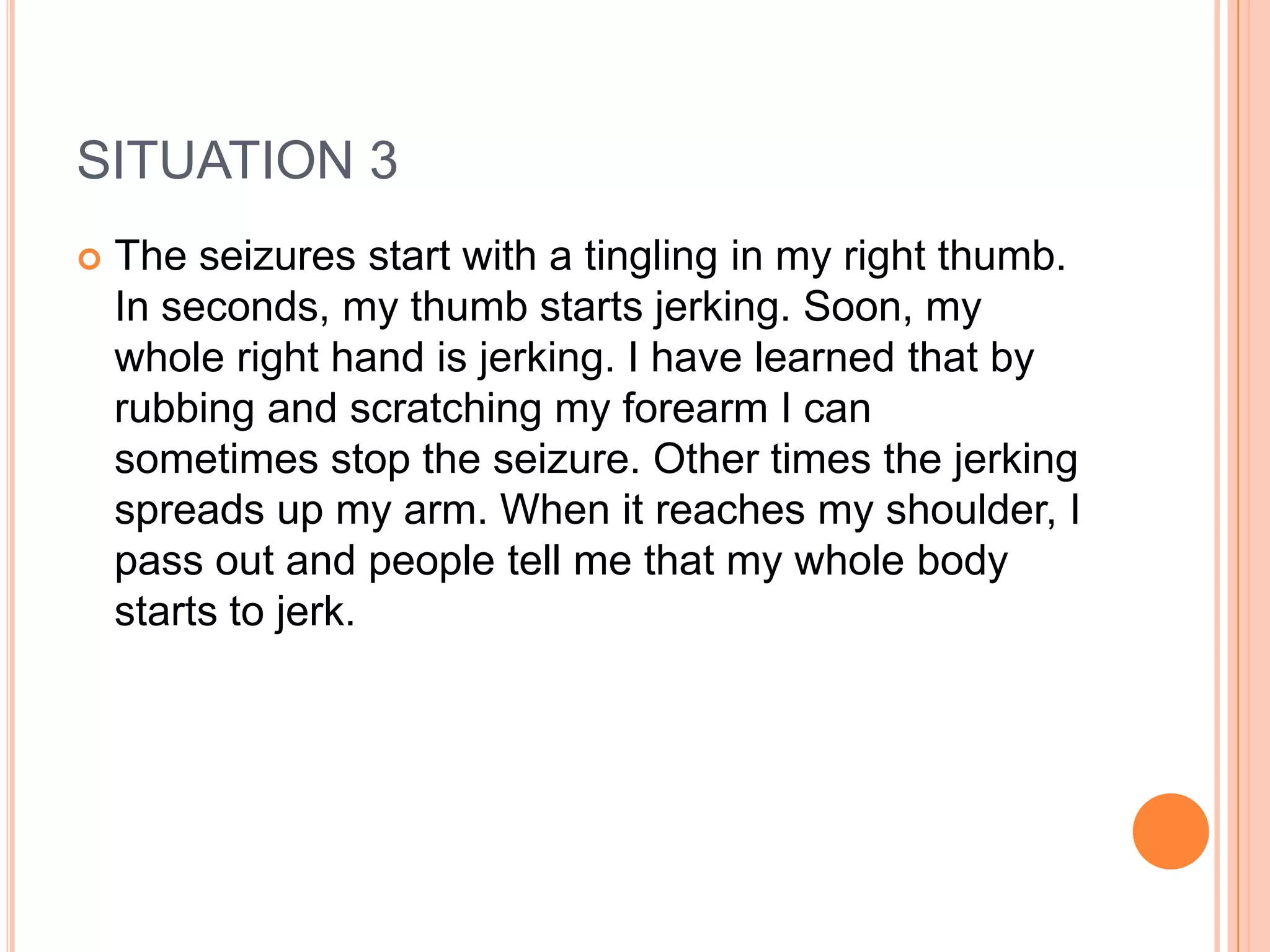
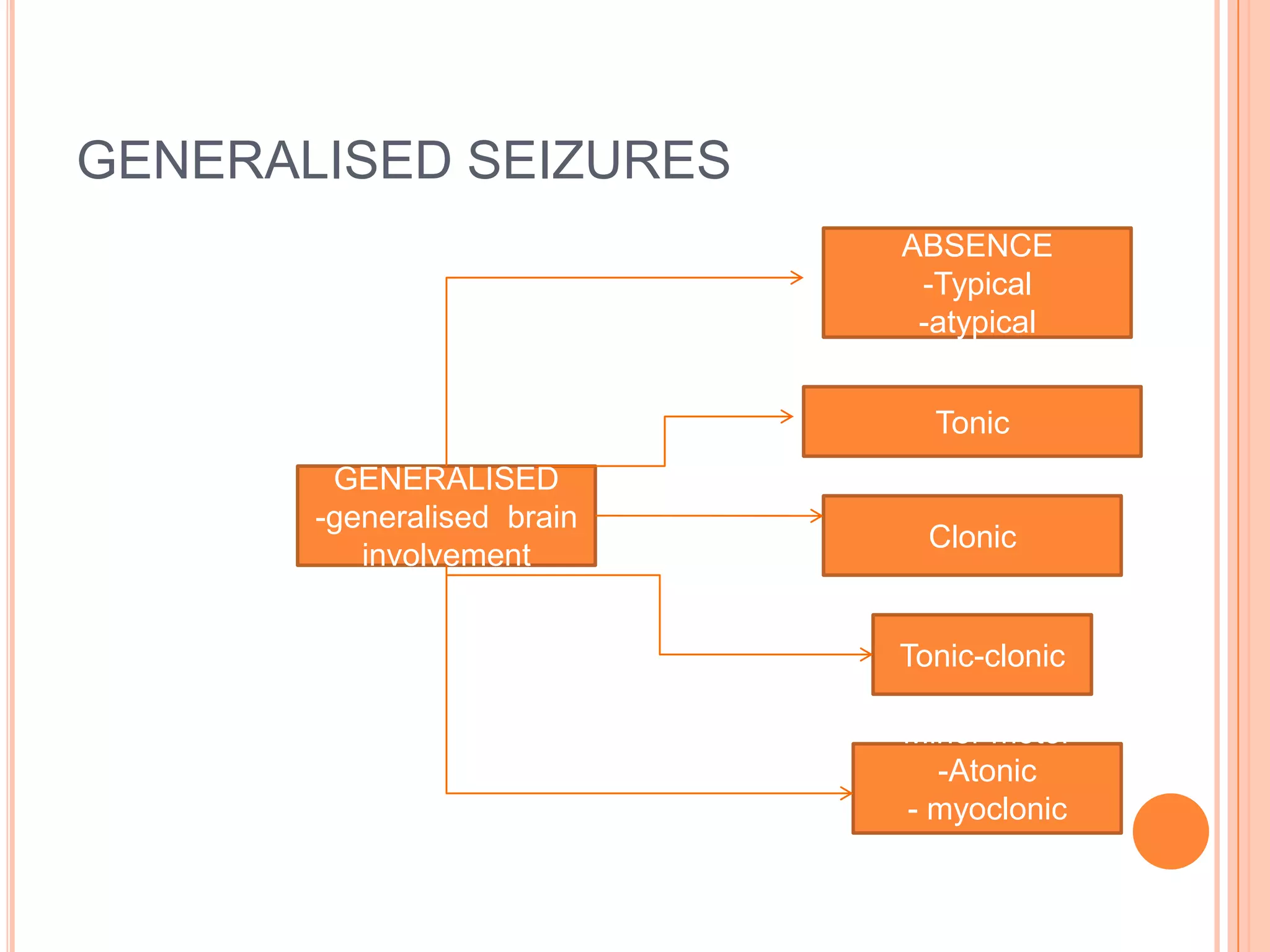
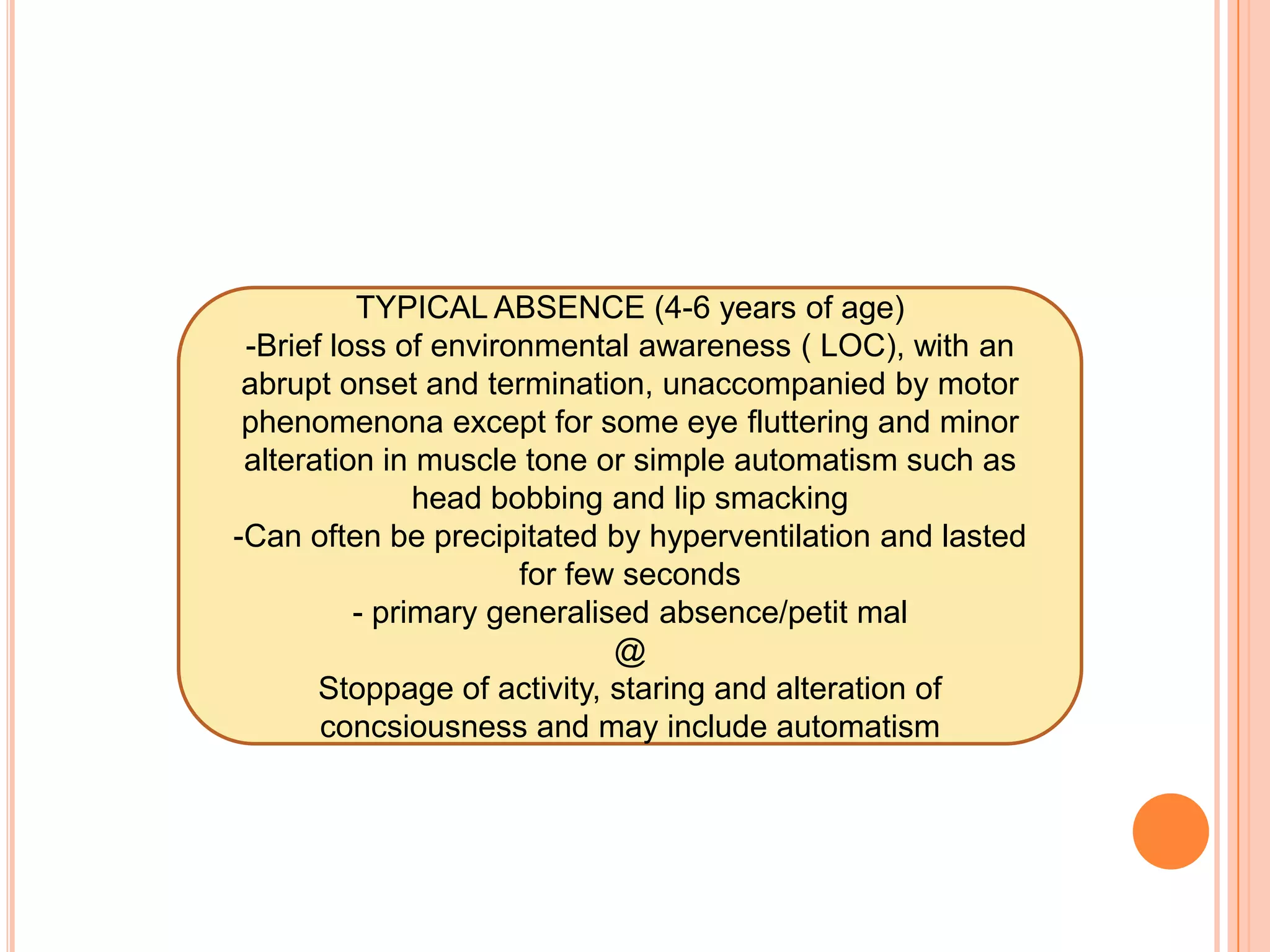
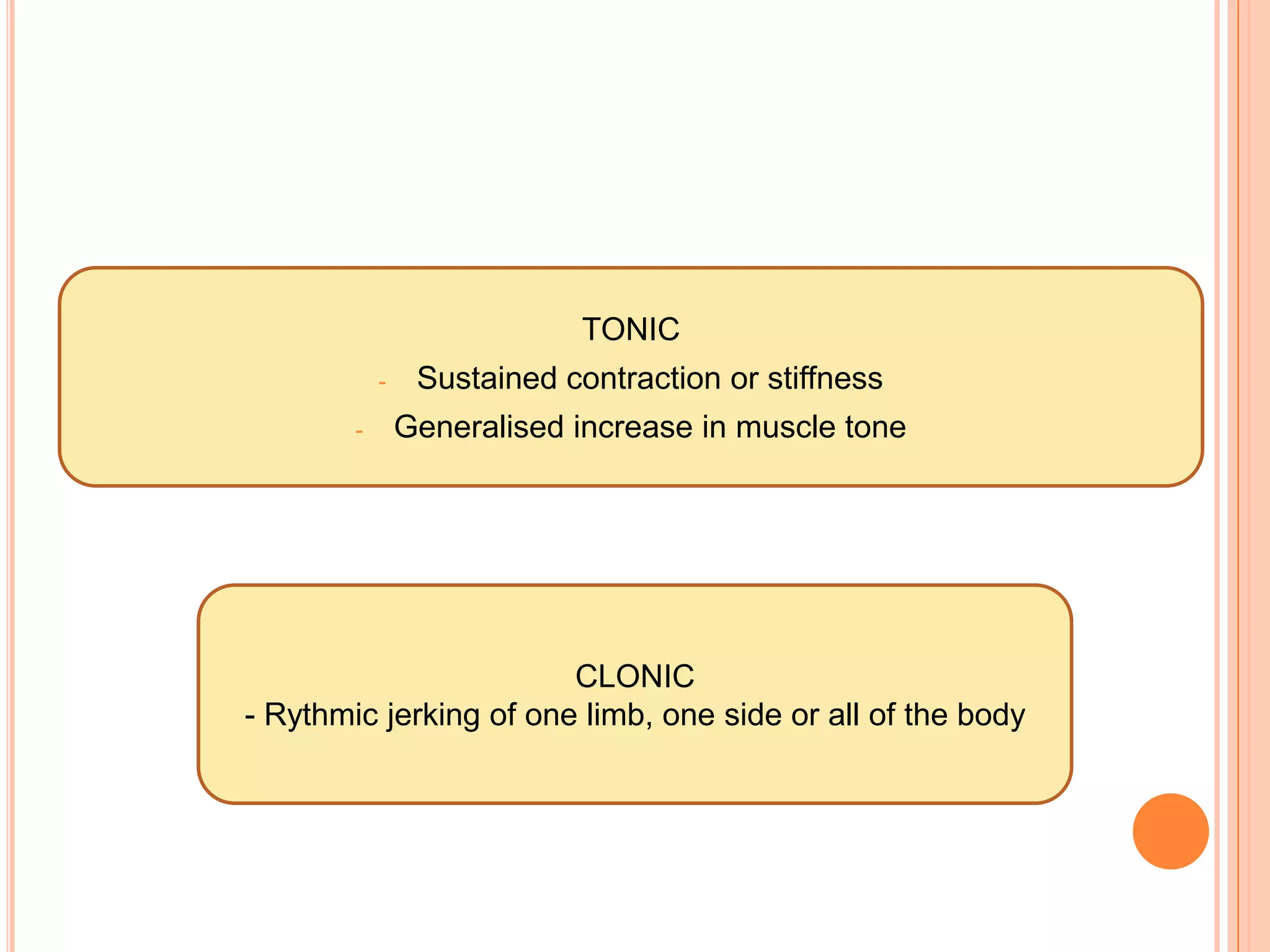
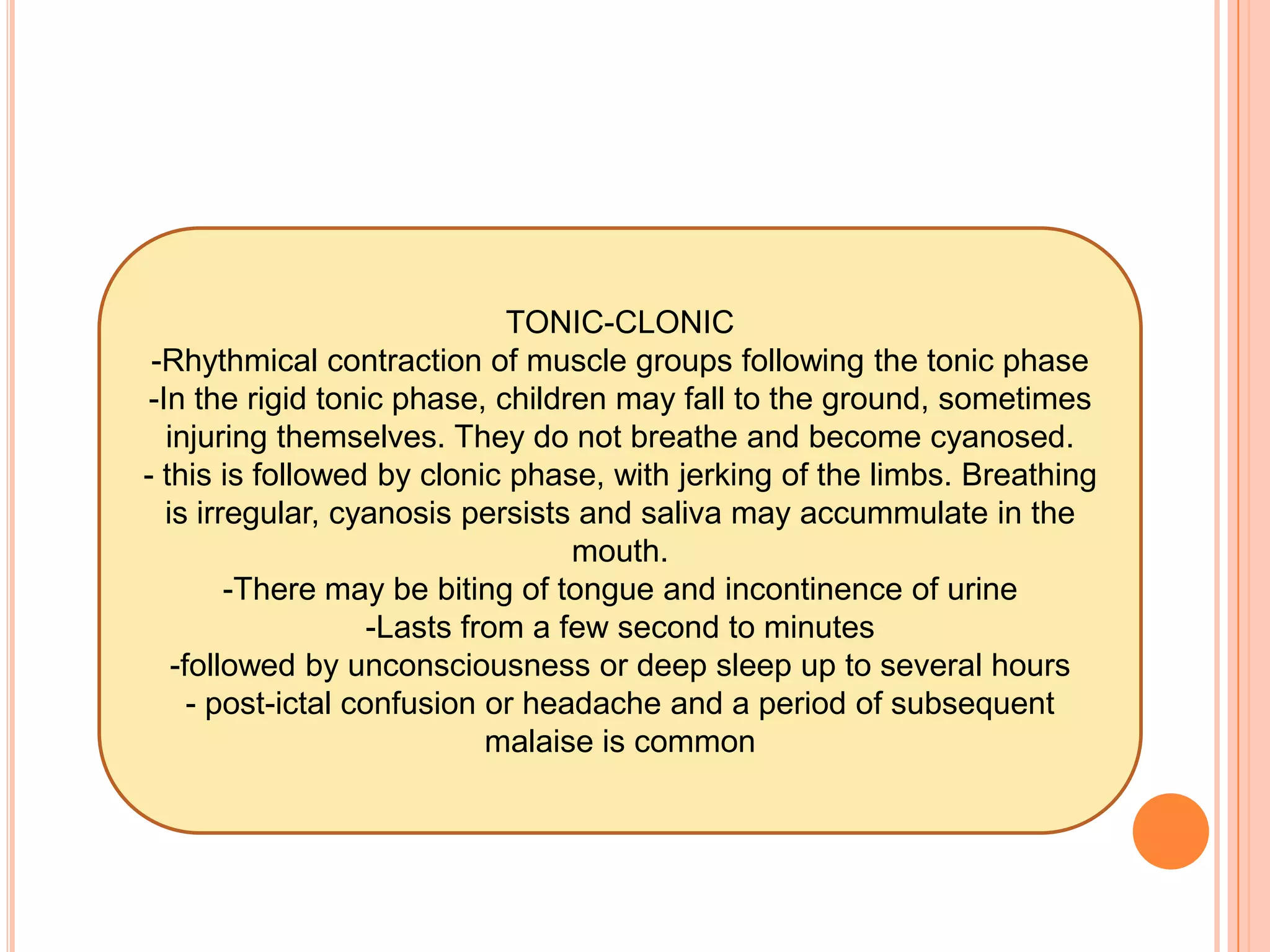
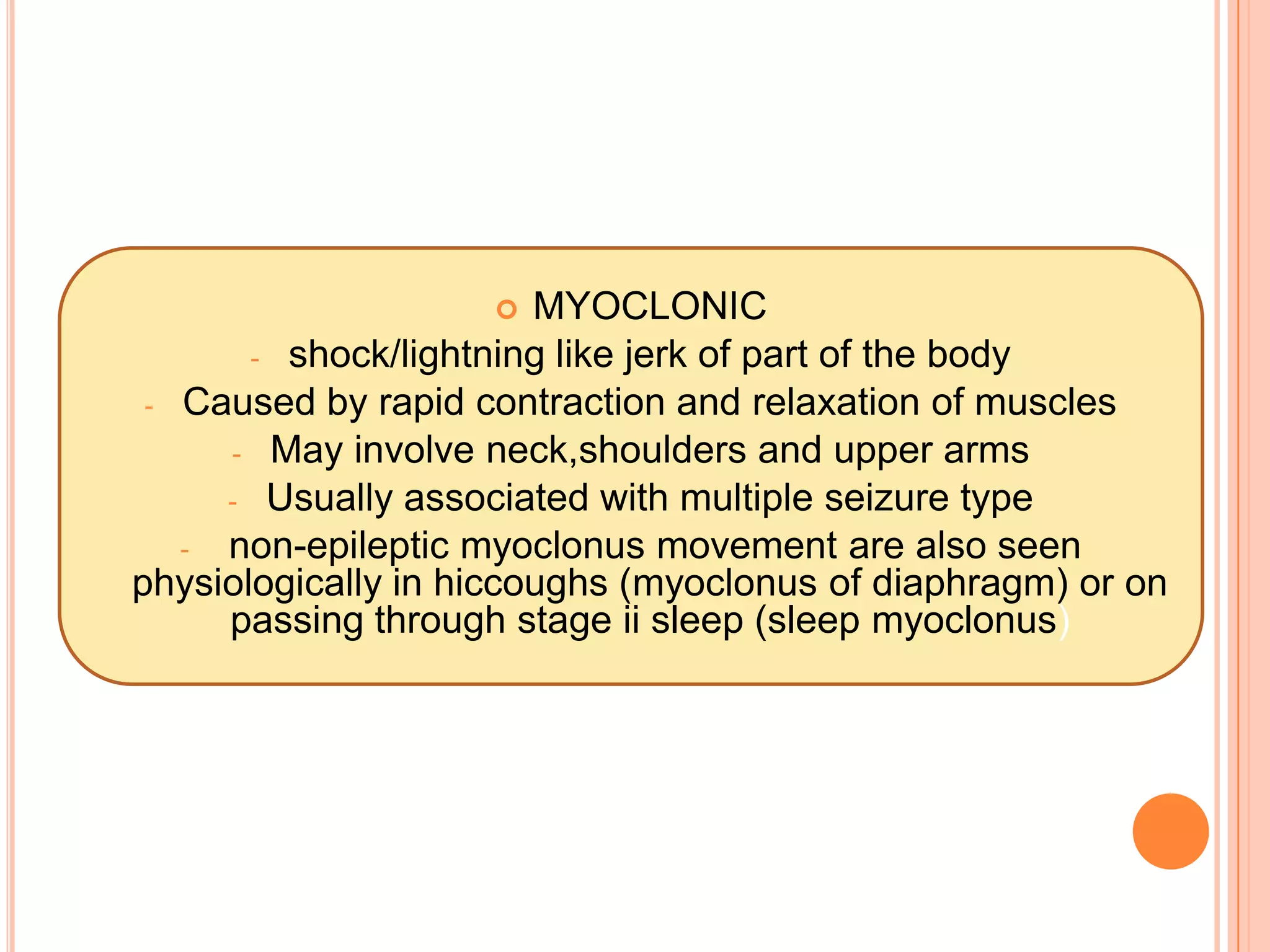
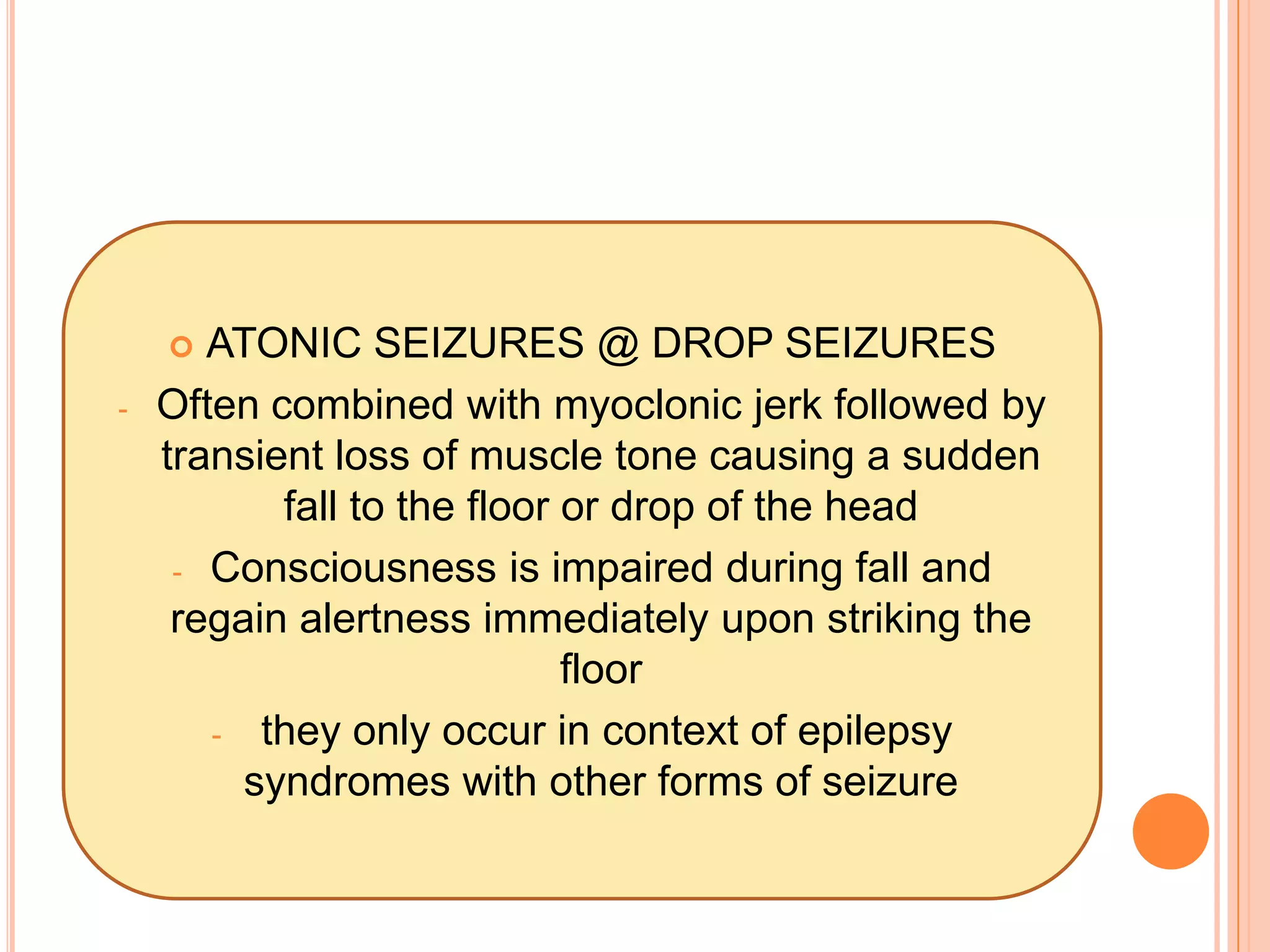
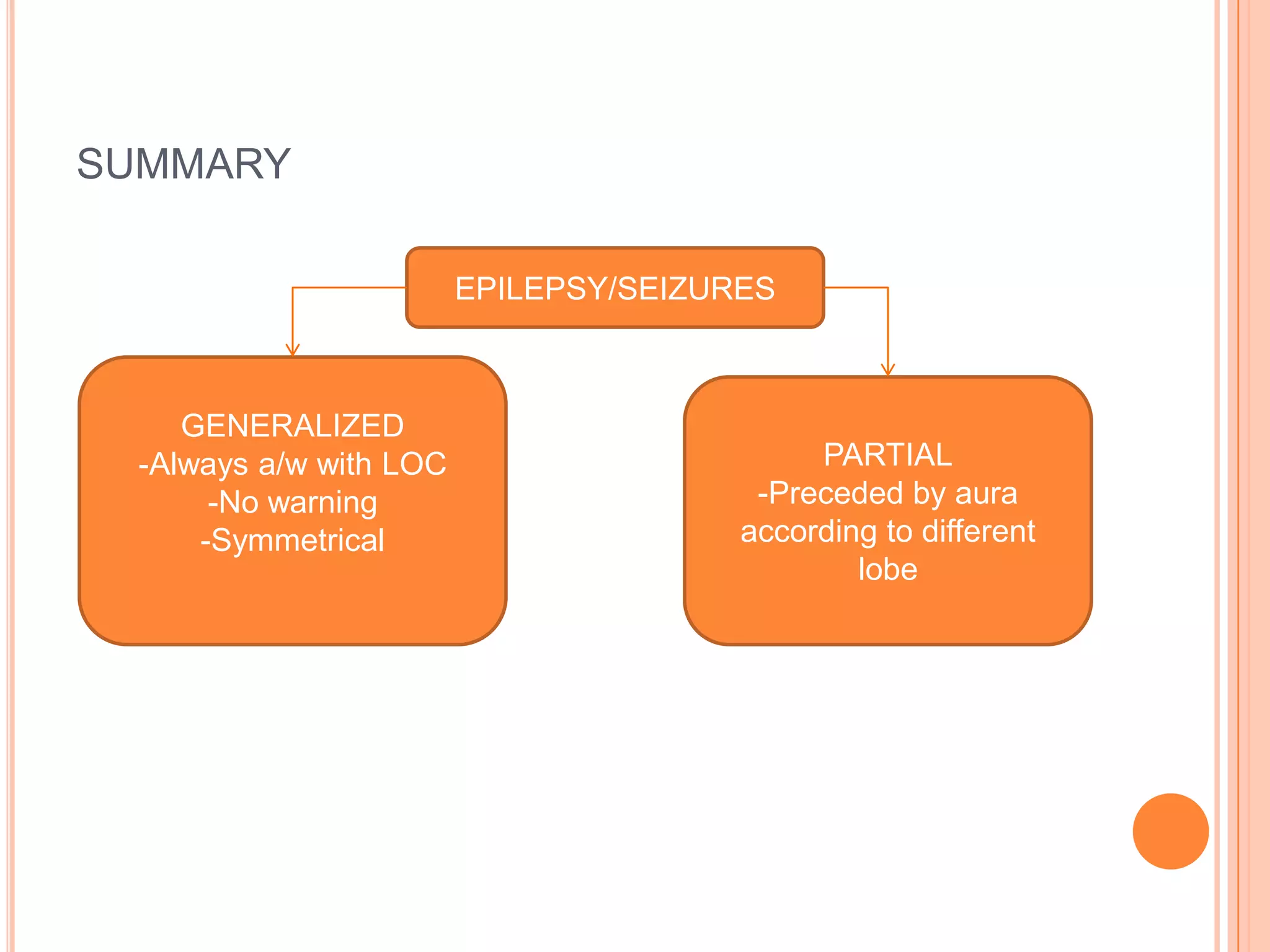
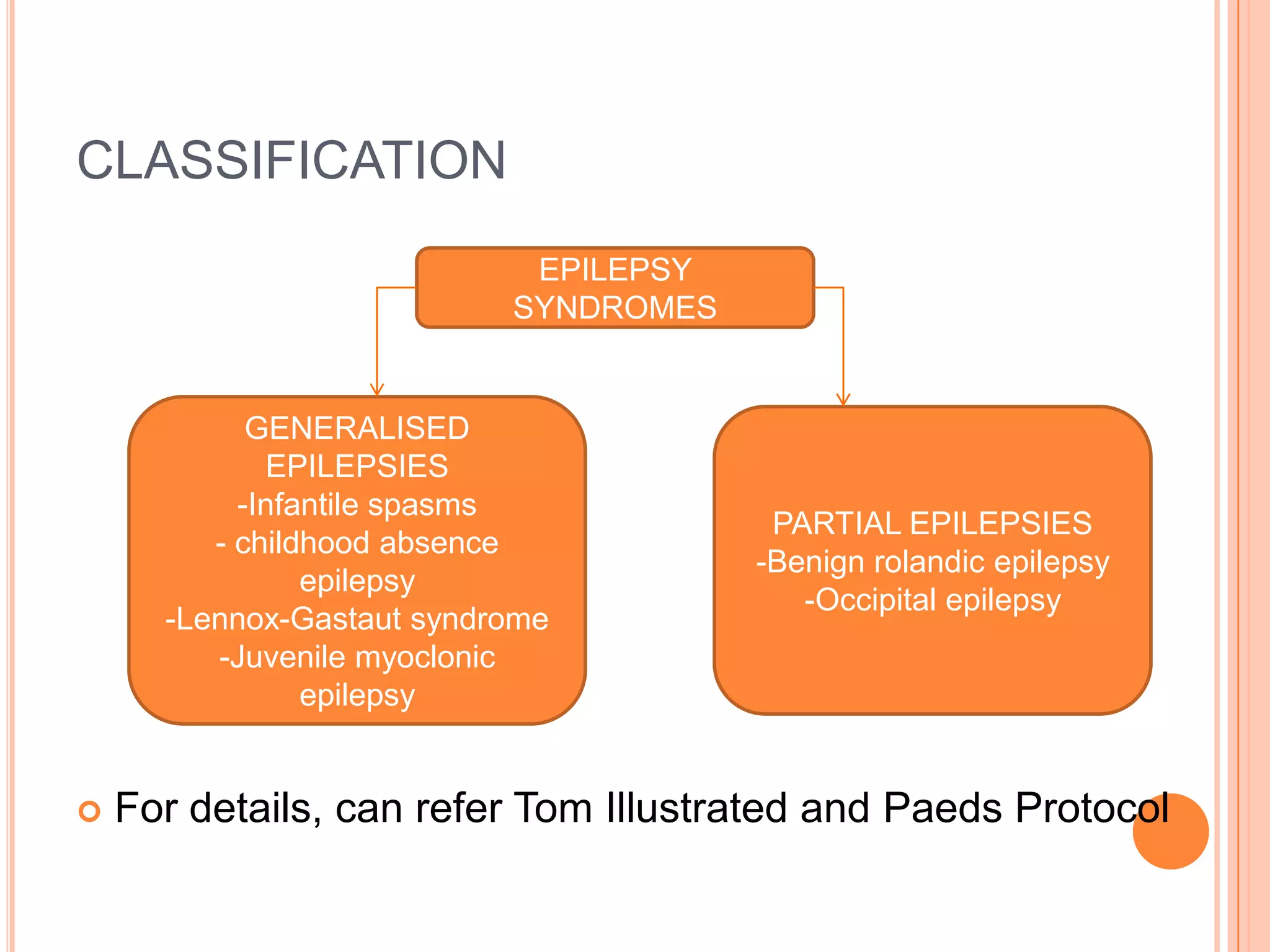
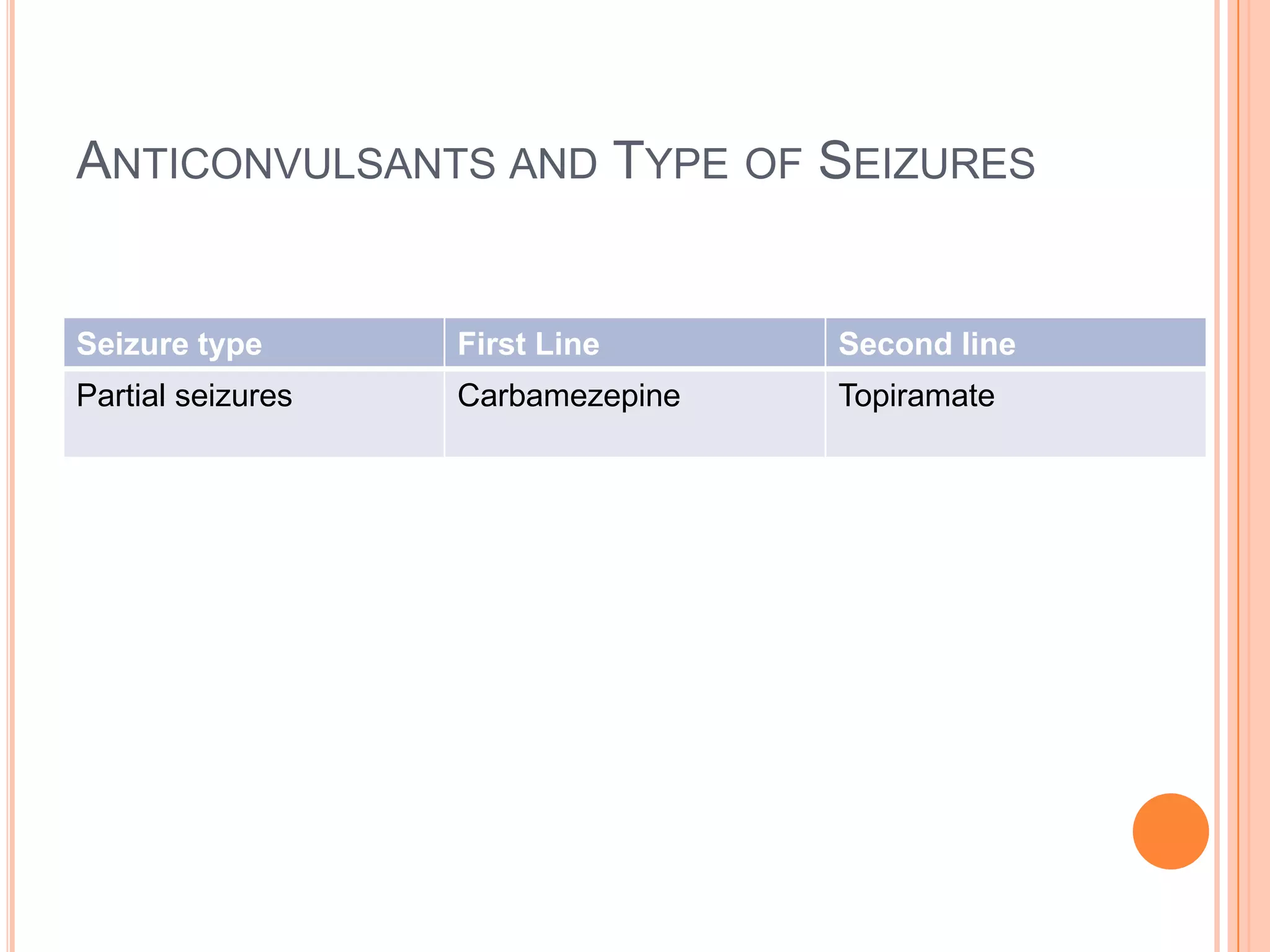
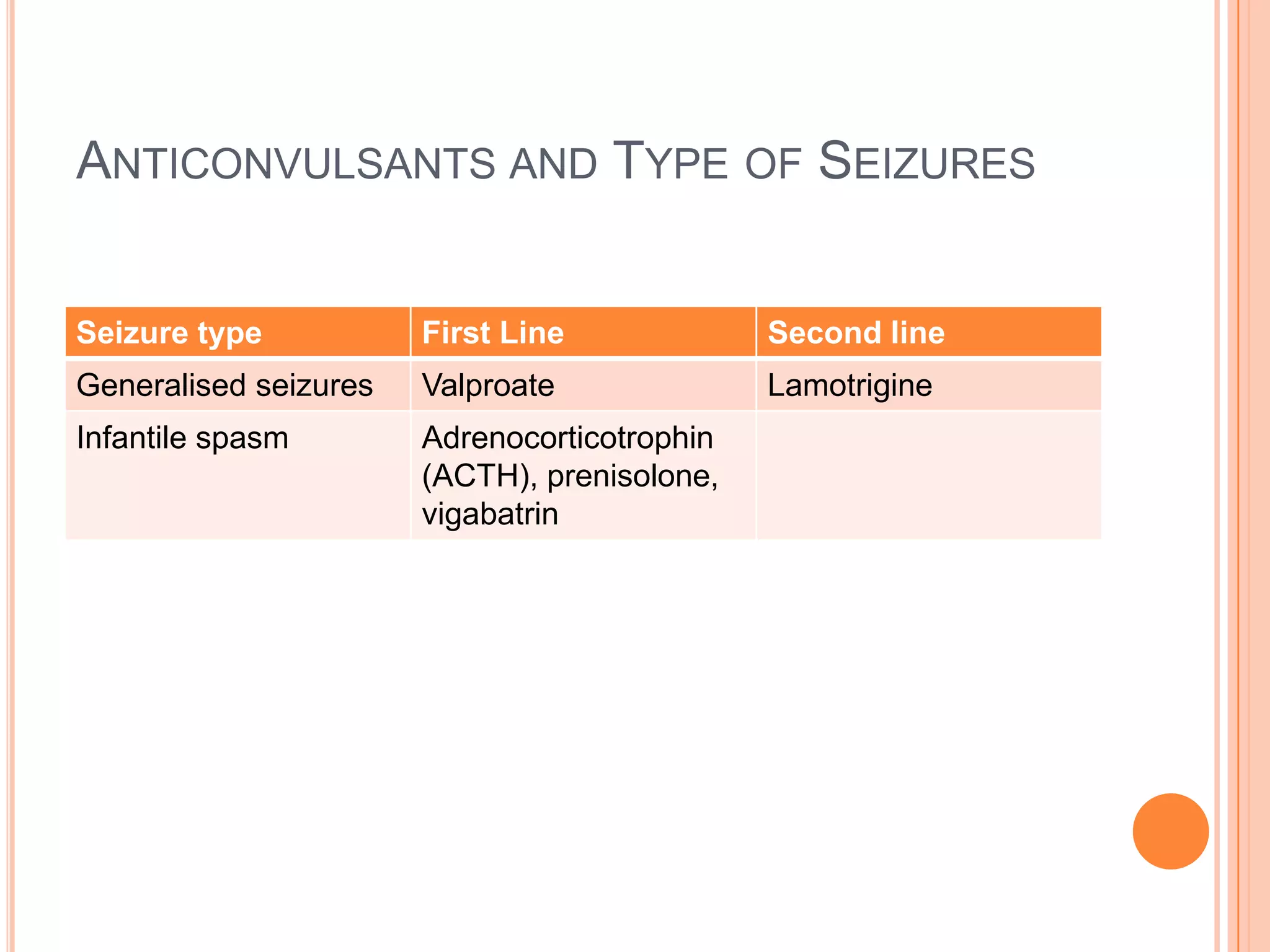
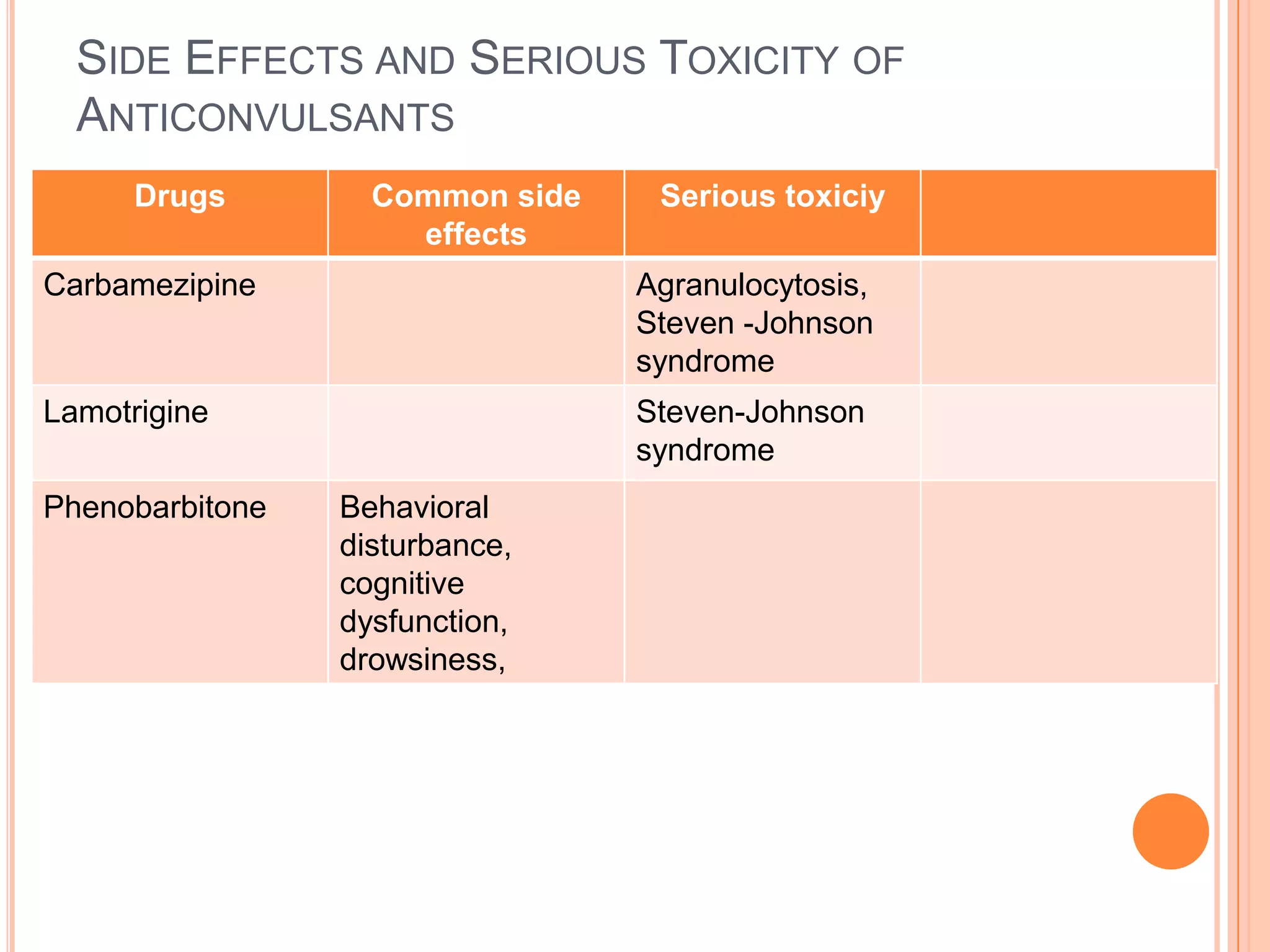
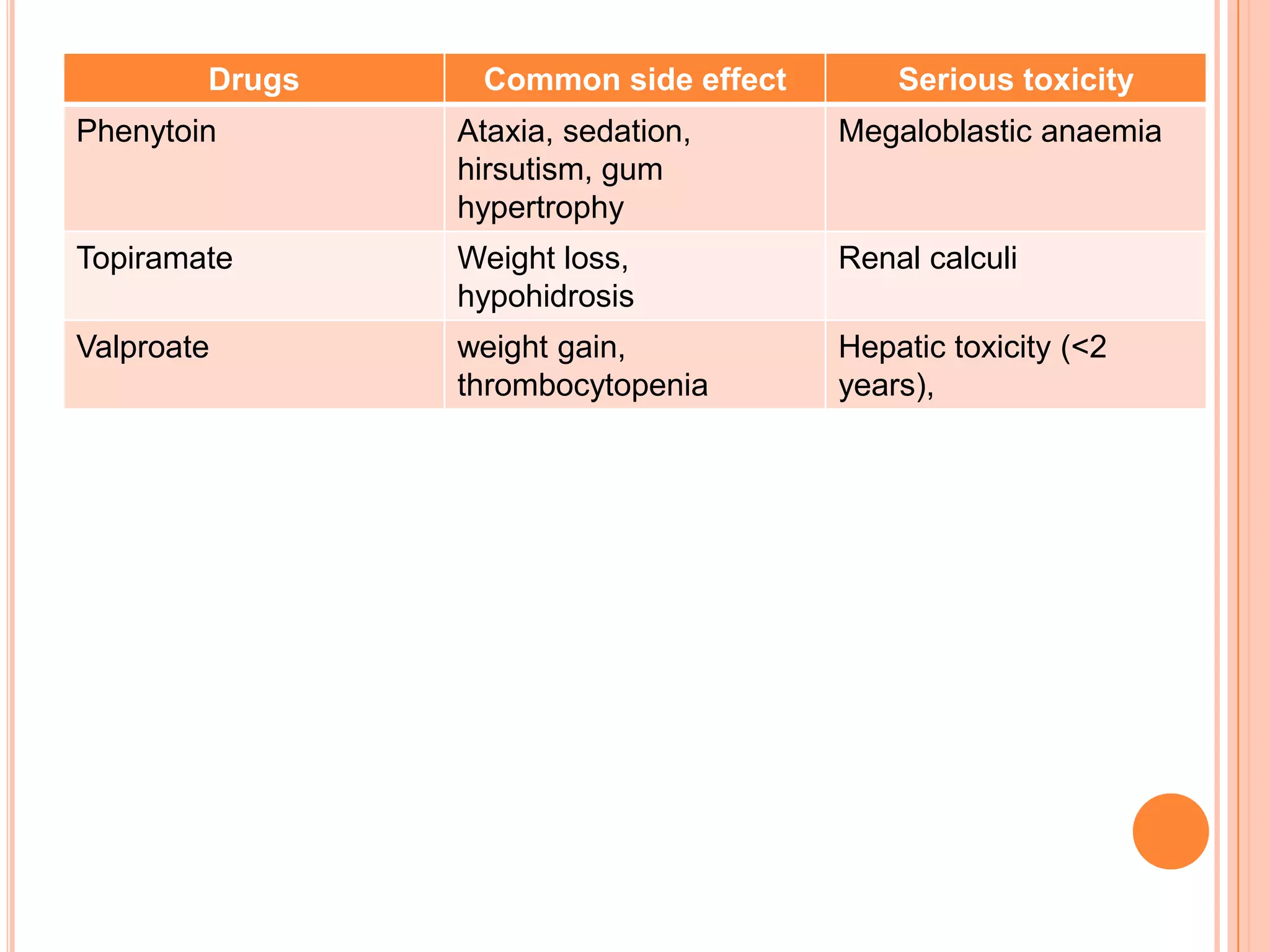
This document defines seizures and epilepsy and describes different types of seizures. It discusses partial and generalized seizures. Partial seizures are further divided into simple and complex seizures. Generalized seizures include absence, tonic, clonic, tonic-clonic, myoclonic and atonic seizures. Various case examples are provided to illustrate the clinical presentation of different seizure types. Risk factors, causes and classification of seizures are also outlined.