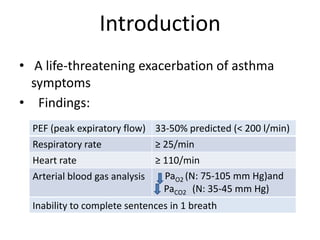
This document provides guidelines for the management of acute severe asthma. Initial assessment involves measuring peak expiratory flow, vital signs, and arterial blood gases. Treatment includes high doses of inhaled bronchodilators, systemic corticosteroids, oxygen, intravenous fluids and magnesium. Mechanical ventilation may be required if the patient deteriorates or is unable to be adequately ventilated. Close monitoring of peak expiratory flow, oxygen saturation, and serum aminophylline levels is important.