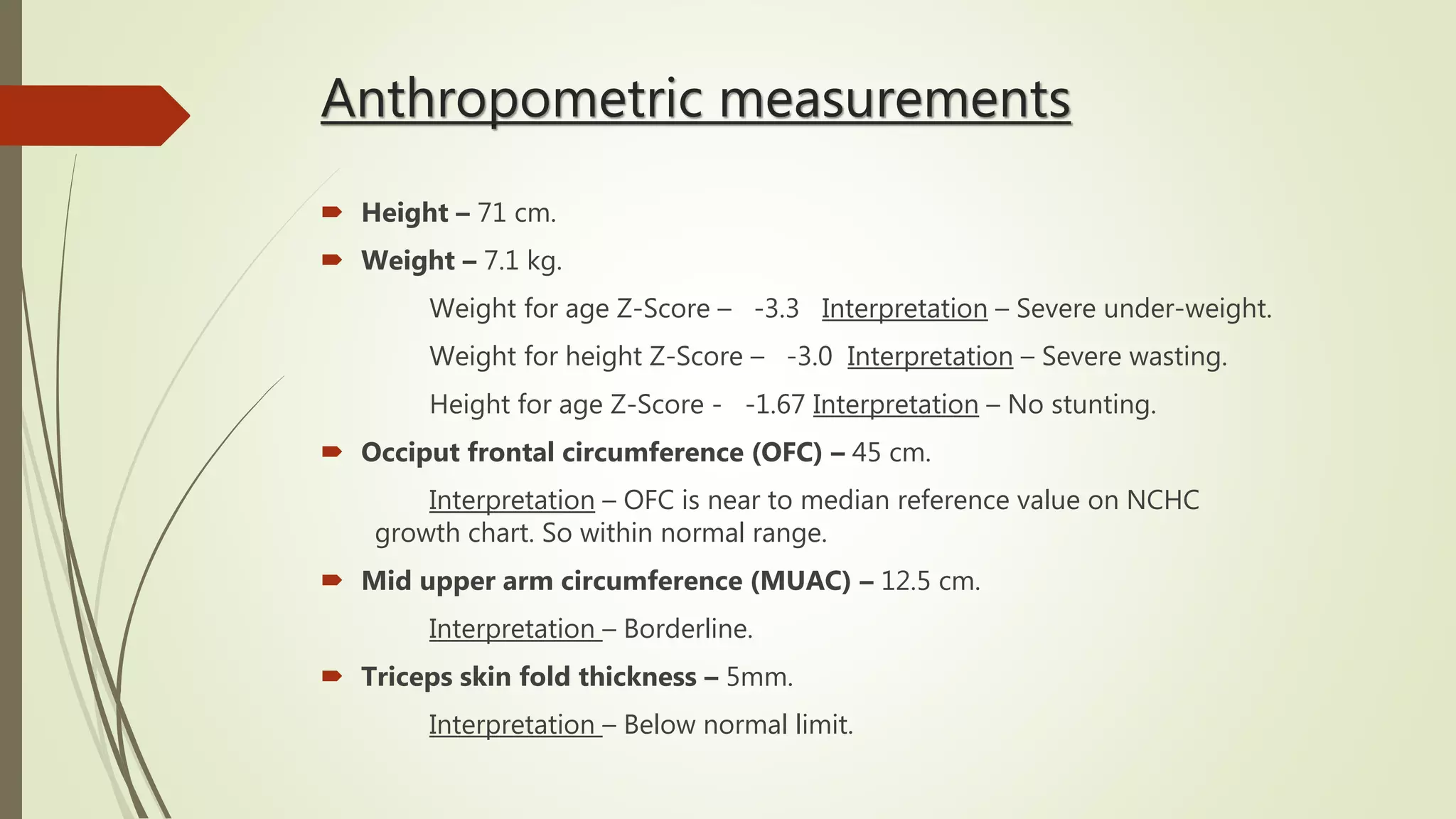
This case presentation describes a 1 year old male patient admitted to the pediatric ward with a 4 day history of fever, cough, runny nose and 2 days of breathlessness. On examination, the patient appeared ill with tachycardia and tachypnea. Chest examination revealed wheezing and crackles. Echocardiogram showed a patent ductus arteriosus. The patient was diagnosed with bronchiolitis and congenital heart disease due to PDA, and was failing to thrive. Treatment included antibiotics, bronchodilators, diuretics and supportive care. The patient's condition was followed up over three days.