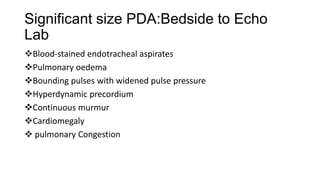
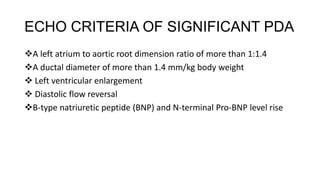
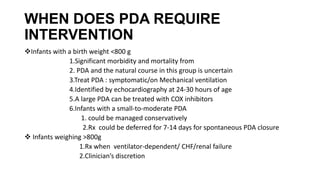
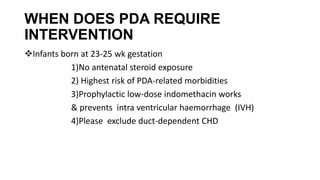
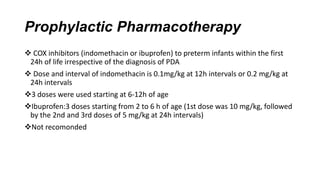
The document discusses the management of patent ductus arteriosus (PDA) in preterm infants. PDA occurs in 31% of very low birth weight infants and can be left untreated in some cases. Treatment may include conservative management, pharmacological closure with drugs like indomethacin or ibuprofen, or surgical ligation if drugs fail. Prophylactic drug treatment may help prevent complications in very preterm infants under 25 weeks gestation. The optimal management of PDA in infants under 800g is still debated, as untreated PDA carries risks but interventions also pose dangers.