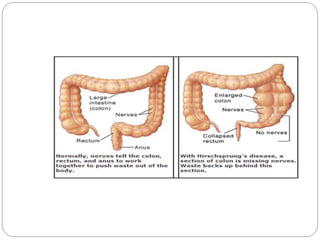
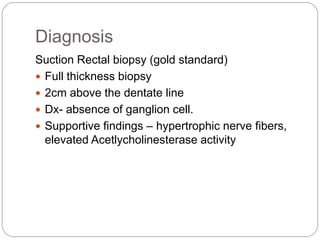
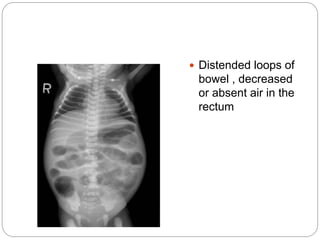
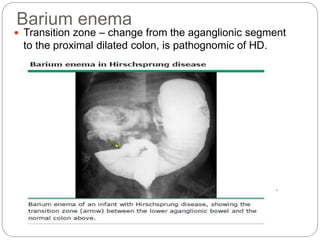
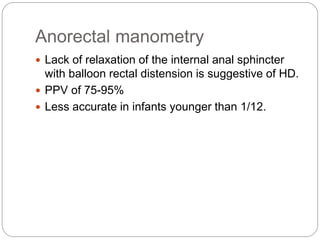
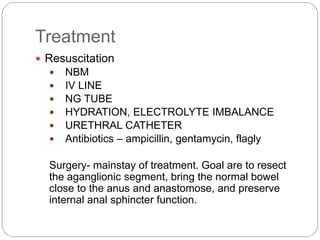
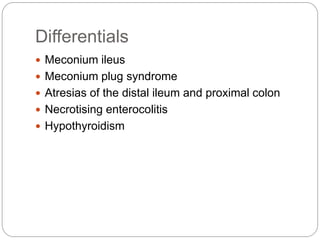
Hirschsprung disease is a developmental disorder characterized by the absence of ganglia in the distal intestine, resulting in functional obstruction. It is caused by a defect in the migration of neural crest cells during development. This leaves the distal intestine unable to relax and pass stool. Symptoms include delayed passage of meconium in newborns and chronic constipation in older children. Diagnosis is made through rectal biopsy showing lack of ganglion cells. Treatment involves surgically removing the aganglionic segment and reconnecting the bowel.