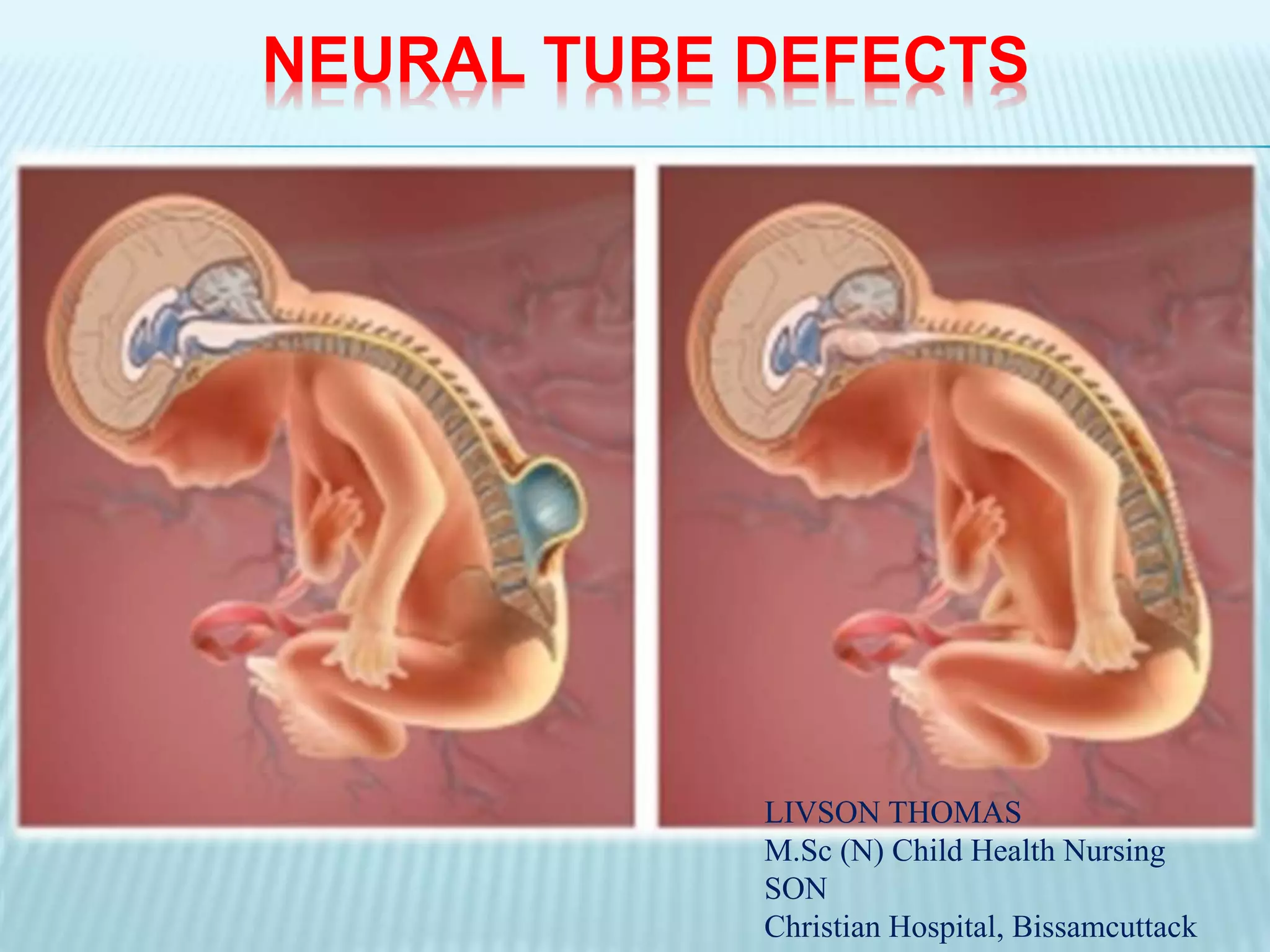
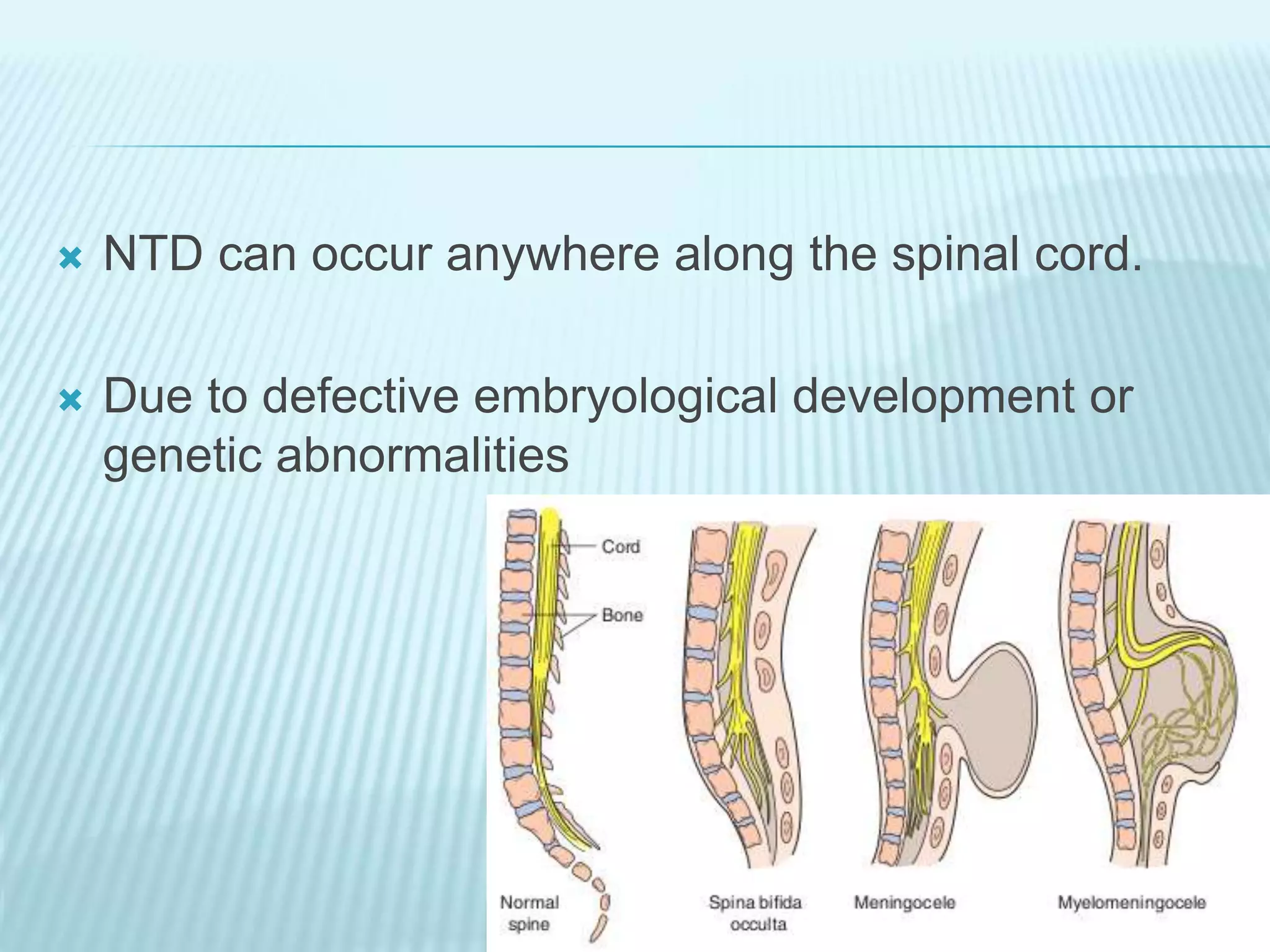
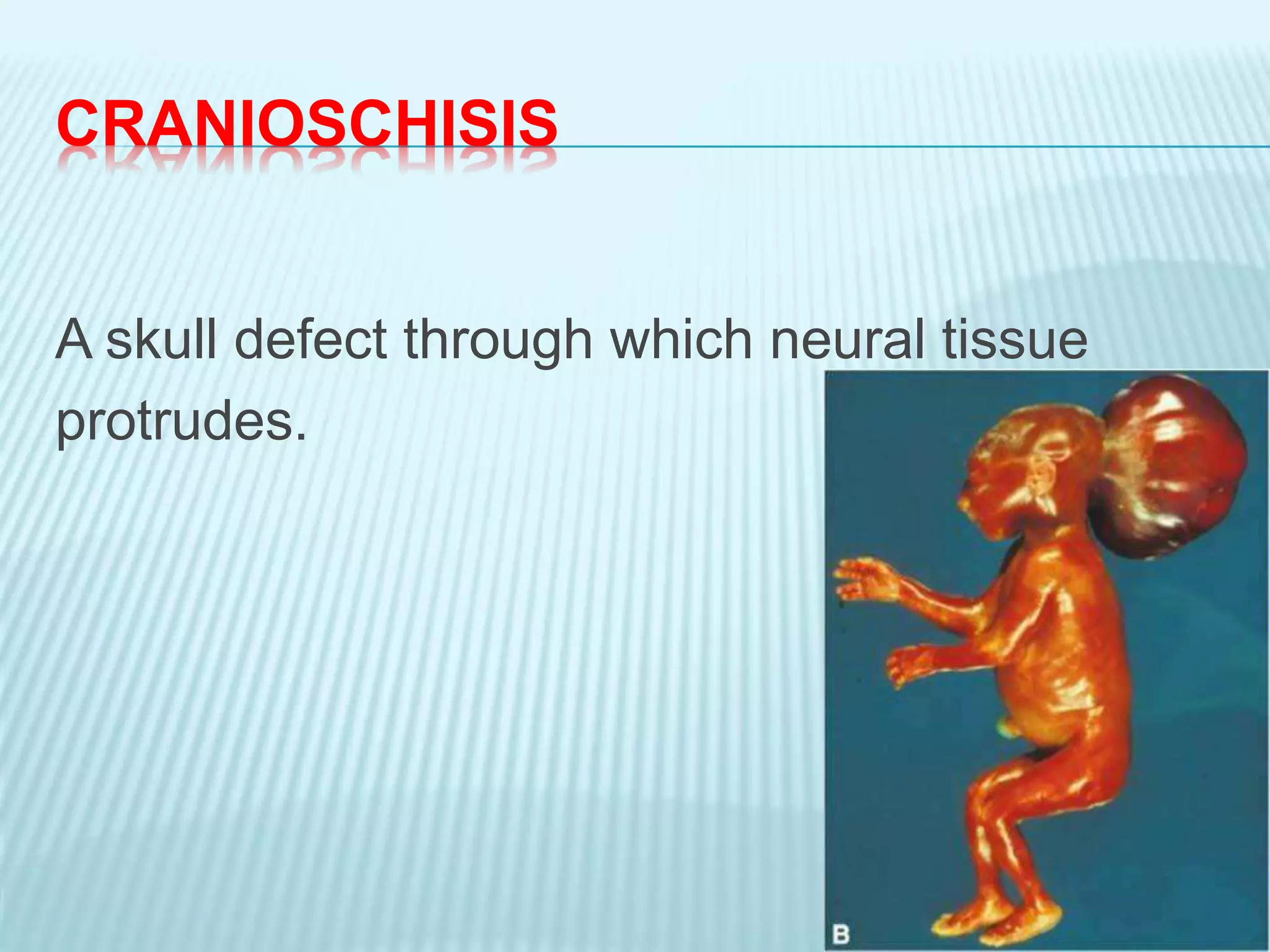
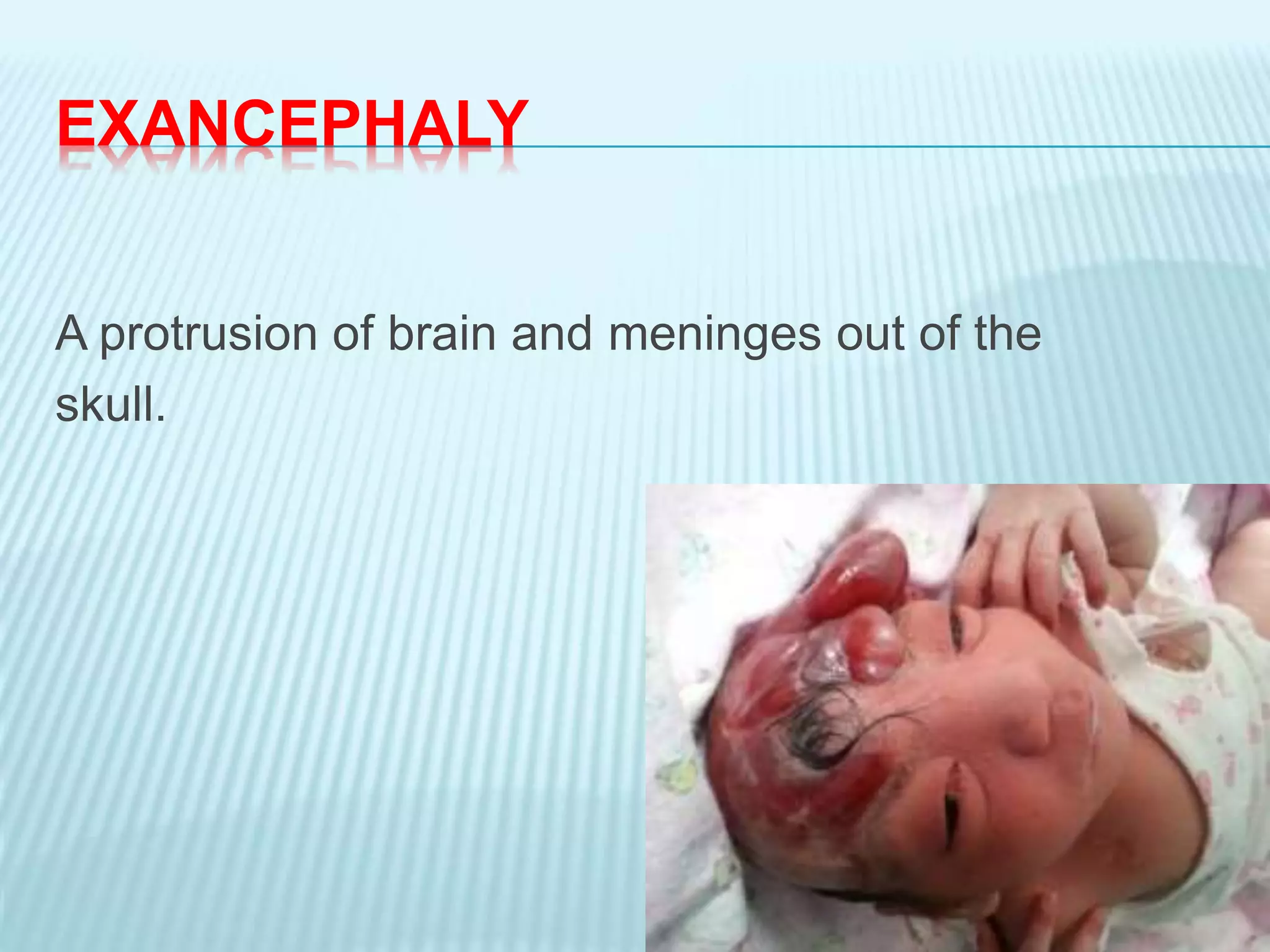
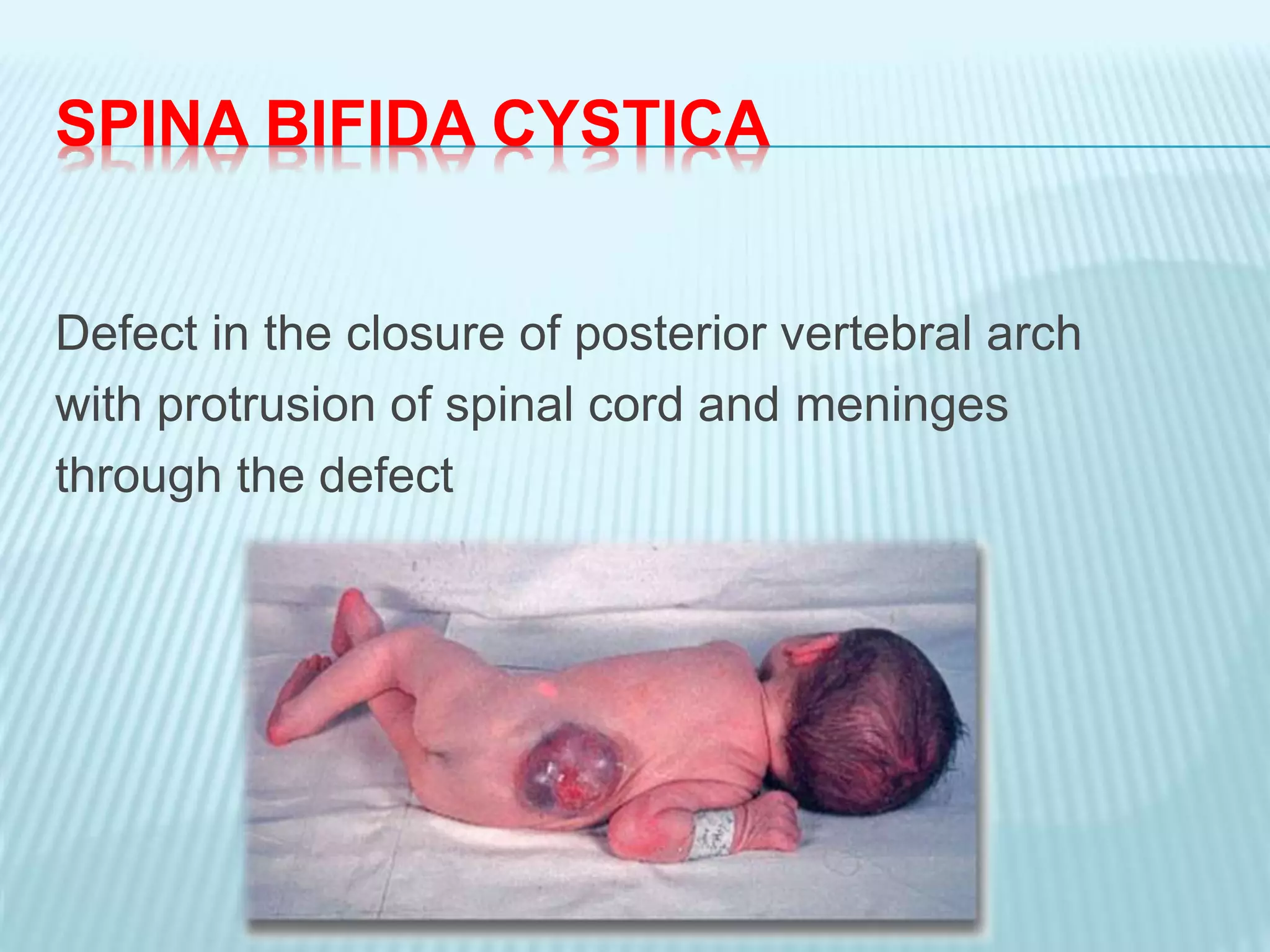
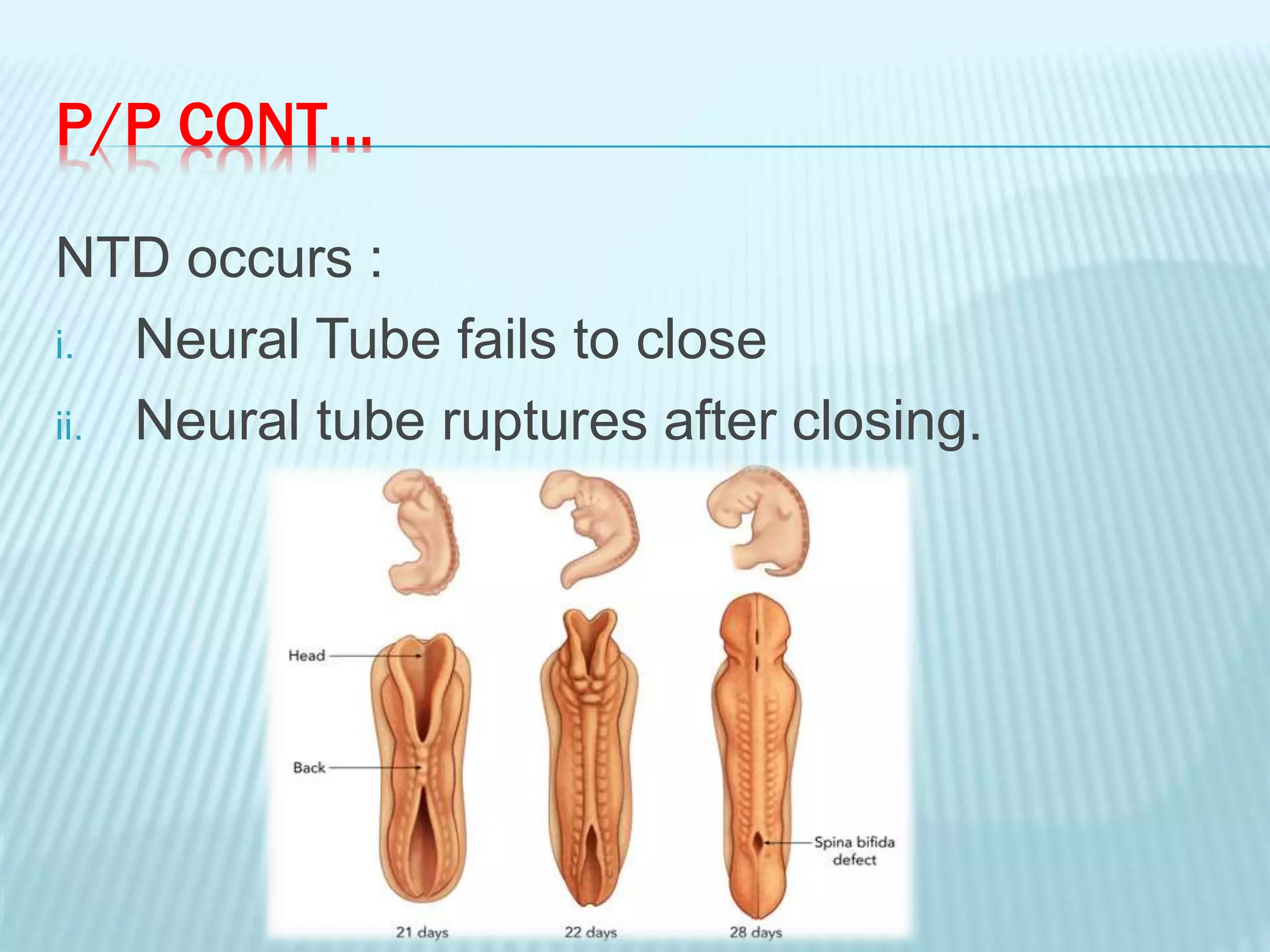
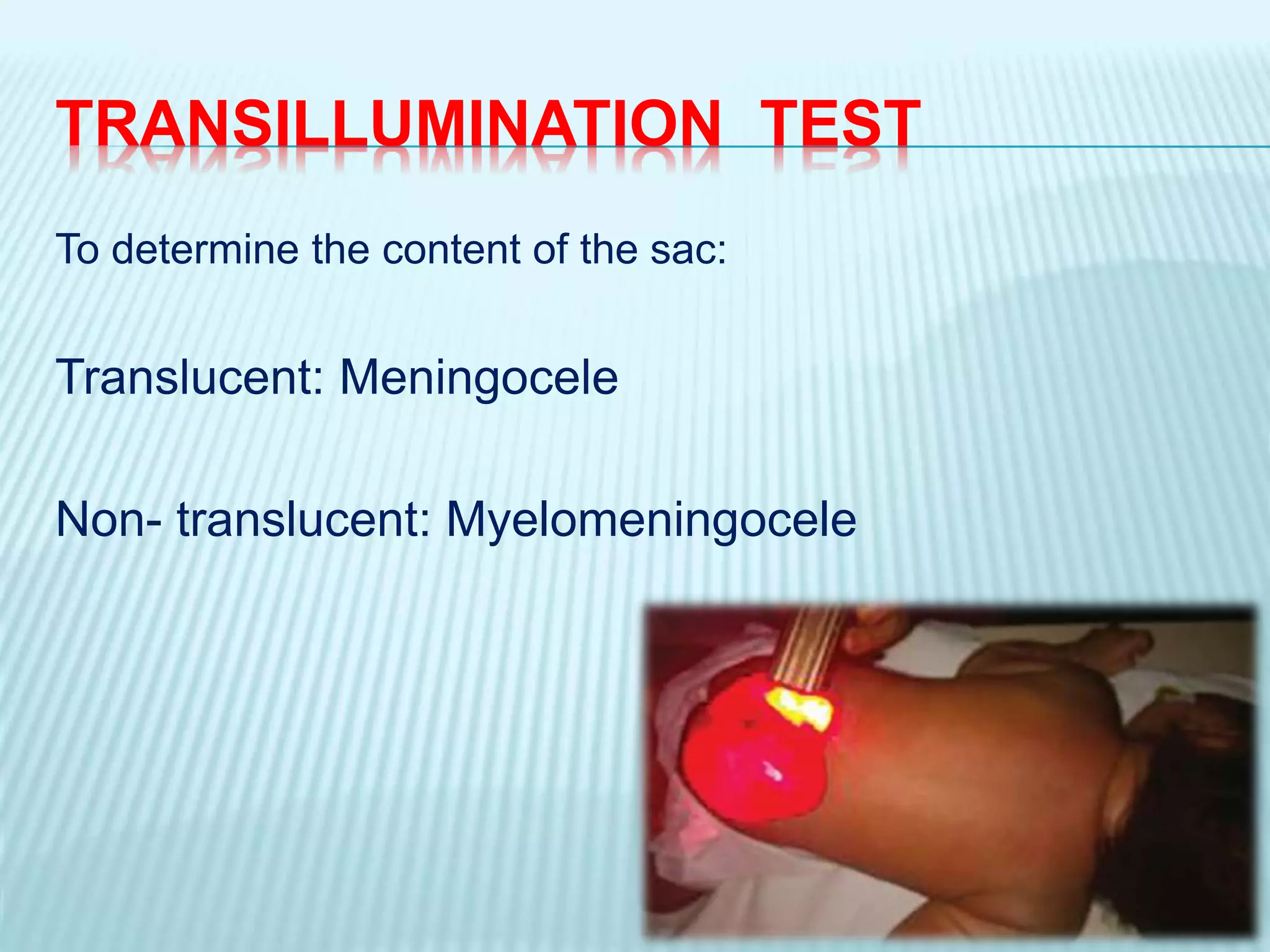
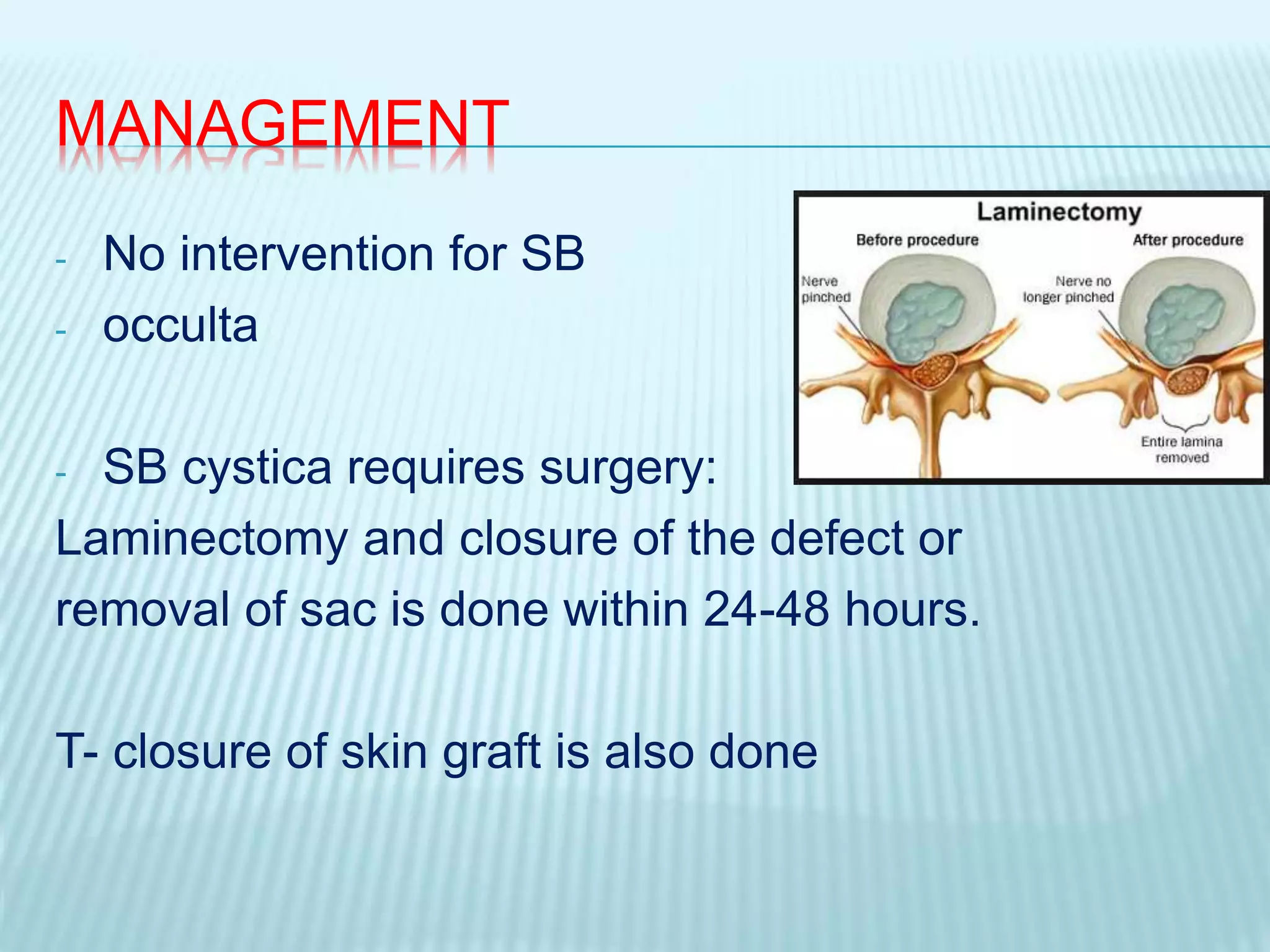
Neural tube defects are birth defects that occur when the spine and brain do not develop properly early in pregnancy. The document discusses several types of neural tube defects including anencephaly, cranioschisis, exencephaly, encephalocele, rachischisis, and spina bifida. Spina bifida is further classified into spina bifida occulta, spina bifida cystica, meningocele, and myelomeningocele. The causes include genetic and environmental factors like folic acid deficiency. Clinical features and management involve surgical closure of defects and prevention of complications. Prognosis depends on location and severity of defect but quality of life can be improved with treatment and care.