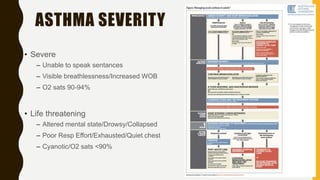
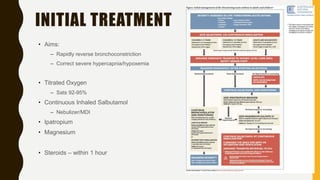
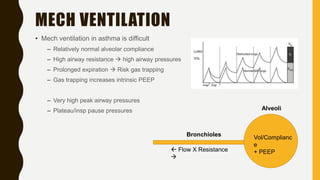
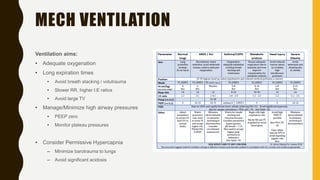
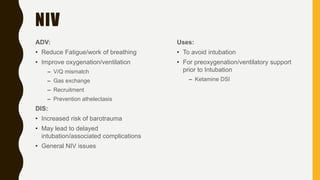
This document discusses the management and ventilation strategies for severe asthma. It describes a case of a 28 year old male presenting with severe asthma exacerbation. Key points include: administering bronchodilators, steroids and magnesium to rapidly reverse bronchoconstriction; considering non-invasive ventilation to reduce workload and improve oxygenation; intubating and using ketamine for induction if exhaustion or respiratory failure occurs; and aiming for long expiratory times and minimal pressures if mechanical ventilation is needed to avoid further lung damage. The case study shows how these treatments were applied and the patient was discharged after intensive care.