This document provides an overview of the management of acute asthma exacerbations. It begins with definitions of asthma and exacerbations. It then covers the epidemiology, pathogenesis, diagnosis, differential diagnosis, assessment, and treatment of acute exacerbations. Treatment involves bronchodilator therapy, anti-inflammatory therapy with corticosteroids, supplemental oxygen, and mechanical ventilation if needed. Goals of mechanical ventilation include maintaining oxygen saturation and minimizing dynamic hyperinflation.

![Pathophysiology
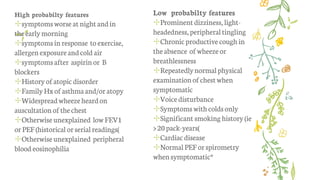
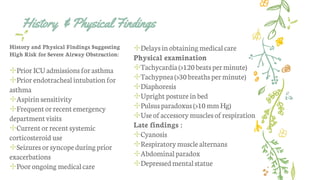
✢The2007 ExpertPanelReport3(EPR-3)oftheNationalAsthma EducationandPreventionProgram(NAEPP)notedseveral
key changesintheunderstandingofthepathophysiology ofasthma[1]
✢Thecritical roleof inflammation hasbeen furthersubstantiated,but evidence is emerging
for considerable variability in thepatternof inflammation,thusindicating phenotypic
differences thatmay influence treatmentresponses
✢Oftheenvironmentalfactors, allergic reactions remainimportant.Evidence alsosuggestsa
keyandexpanding rolefor viral respiratoryinfections in these processes
✢Theonsetof asthmafor mostpatientsbegins early inlife, with thepatternof disease
persistencedeterminedby early,recognizable riskfactors including atopic disease,recurrent
wheezing,anda parentalhistory of asthma
✢Currentasthmatreatmentwithanti-inflammatory therapydoes notappear toprevent
progression oftheunderlying diseaseseverity](https://image.slidesharecdn.com/acutesevereasthma-170712152830/85/Acute-severe-asthma-7-320.jpg)

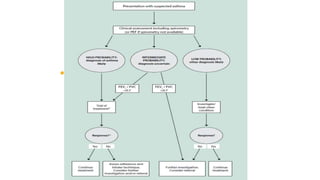
![✢Spirometry is the preferred initial test to assess the
presence and severity of airflow obstruction
Obtainan objective measureofmaximalexpiratoryairflowto
assesstheseverityofobstructionwhenever possible (peak expiratory
flow rate [PEFR]orforcedexpiratoryvolumein1 second [FEVl]).
PEFR (or FEV l ) <40% o f baseline is severe obstruction.](https://image.slidesharecdn.com/acutesevereasthma-170712152830/85/Acute-severe-asthma-11-320.jpg)