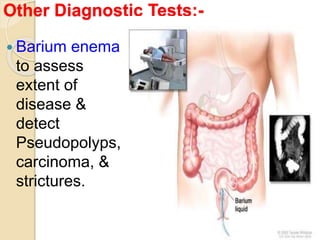
Ulcerative colitis is a chronic inflammatory disease affecting the colon and rectum, with peak incidence in individuals aged 30-50 and complications including a higher risk of colorectal cancer. Diagnosis involves a combination of lab tests, imaging, and endoscopic evaluations, while treatment may include medications such as sulfasalazine and, in severe cases, surgical interventions. Nursing management focuses on symptom relief, fluid balance, nutritional support, and psychological care for affected patients.