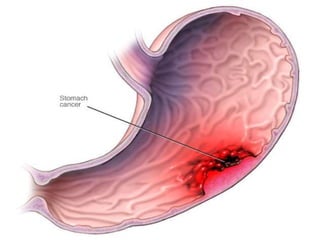
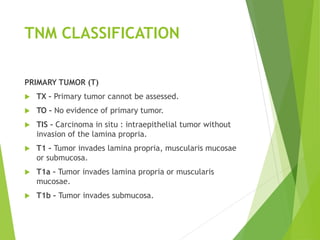
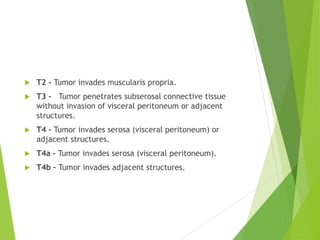
The document discusses gastric cancer, a form of malignant lesions in the stomach, primarily caused by Helicobacter pylori infection and more common in men. It outlines the classification, clinical manifestations, diagnostic evaluation, and management strategies, including chemotherapy, radiation, and surgical options such as gastrectomy. Additionally, it emphasizes the importance of nursing management in preoperative and postoperative care to reduce pain and anxiety and ensure nutritional balance.