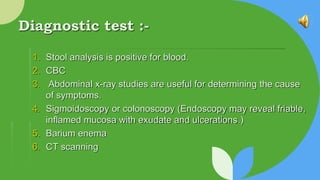
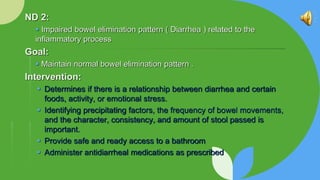
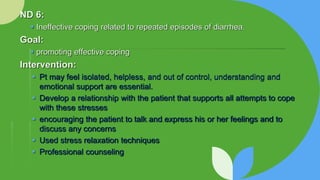
This document provides information on ulcerative colitis (UC) including objectives, pathophysiology, clinical manifestations, diagnostic tests, complications, medical management, nutritional therapy, pharmacologic therapy, indications for surgery, and the nursing process. The objectives are to understand UC pathophysiology, identify diagnostic tests for UC, and formulate nursing care. UC is an inflammatory disease of the colon and rectum characterized by ulcers, inflammation, and bleeding of the mucosa. Diagnostic tests include stool analysis, imaging, and endoscopy. Complications include toxic megacolon. Treatment involves reducing inflammation, immunosuppression, nutrition support, and sometimes surgery. The nursing process addresses pain, bowel dysfunction, nutrition, skin integrity, coping,