This document provides an overview of acid-base physiology, including:
- Definitions of acids, bases, and acid-base balance
- The three main systems that maintain pH balance: buffers, respiration, and renal
- The four basic types of acid-base imbalances: metabolic acidosis, metabolic alkalosis, respiratory acidosis, respiratory alkalosis
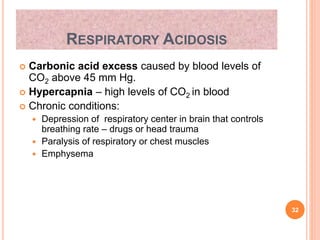
- Details on specific disorders like respiratory acidosis, metabolic acidosis, and mixed disorders
- Compensatory responses and interpretation of blood gas measurements
- Case studies on mixed disorders involving respiratory and metabolic components
In under 3 sentences, it summarizes key concepts in acid-base physiology and provides examples of interpreting acid-base imbalances.















![HENDERSON-HASSELBACH EQUATION
pH = pKa + log([HCO3
-]/.03xpCO2)
Shows that pH is a function of the ratio between
bicarbonate and pCO2
PCO₂ - ventilatory parameter (40 +/- 4)
HCO₃⁻ - metabolic parameter (22-26 mmol/L)
3
2
24
HCO
PaCO
H
Kassirer-Bleich equation
16](https://image.slidesharecdn.com/acidbasedisordersstmu-150611044016-lva1-app6891/85/Acid-base-disorders-stmu-16-320.jpg)


![SAMPLE ANALYSIS
The blood gas machines in most labs actually
measure the pH ,the pCO2 and the pO2.
bicarbonate level -------- from a serum sample.
The [HCO3-] and the base difference are calculated
values using the Henderson-Hasselbalch equation.
19](https://image.slidesharecdn.com/acidbasedisordersstmu-150611044016-lva1-app6891/85/Acid-base-disorders-stmu-19-320.jpg)





![ACID BASE DISORDERS
Disorder pH [H+] Primary
disturbance
Secondary
response
Metabolic
acidosis
[HCO3
-] pCO2
Metabolic
alkalosis
[HCO3
-] pCO2
Respiratory
acidosis
pCO2 [HCO3
-]
Respiratory
alkalosis
pCO2 [HCO3
-]
25](https://image.slidesharecdn.com/acidbasedisordersstmu-150611044016-lva1-app6891/85/Acid-base-disorders-stmu-25-320.jpg)























![HYPOALBUMINEMIA
In this step interpreting metabolic acidosis is
adjusting for factors that would falsely lower the
anion gap if one existed, e.g.,
hypoalbuminemia and lithium
or bromide ingestion
Adjusted AG in hypoalbuminemia = observed AG +
[2.5(normal albumin − observed albumin)].
50](https://image.slidesharecdn.com/acidbasedisordersstmu-150611044016-lva1-app6891/85/Acid-base-disorders-stmu-50-320.jpg)






