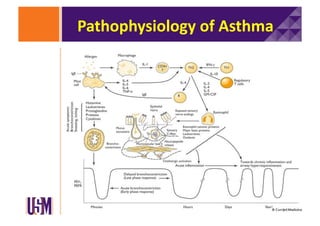
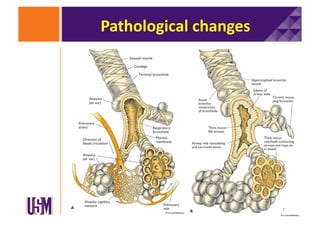
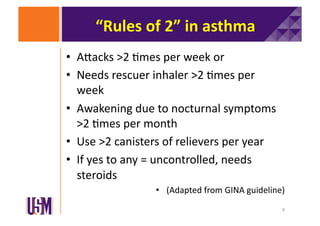
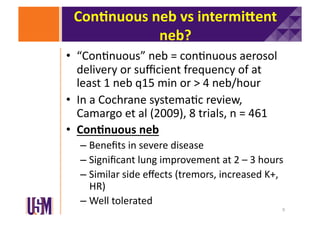
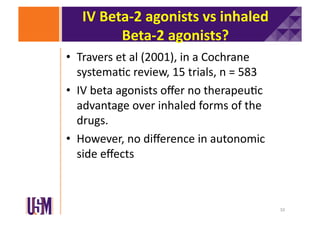
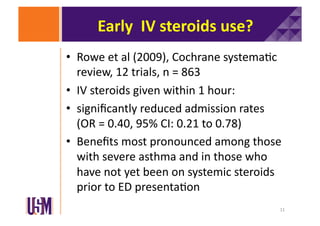
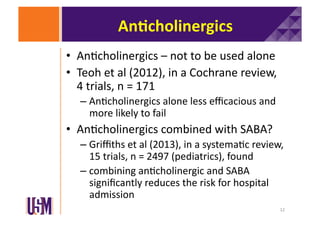
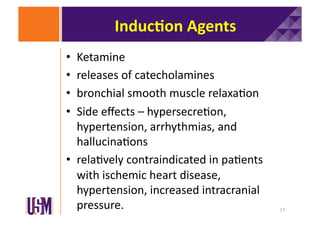
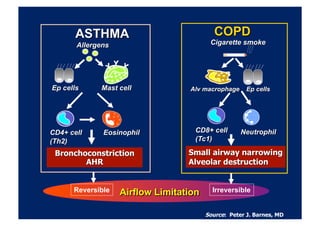
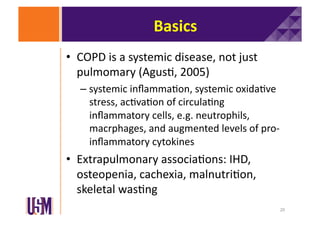
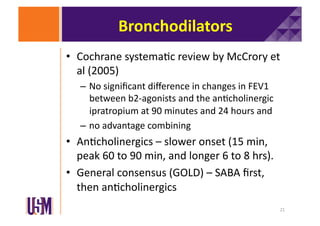
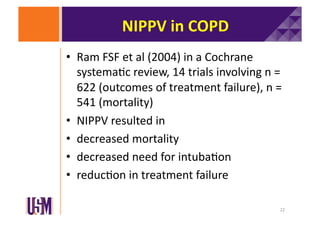
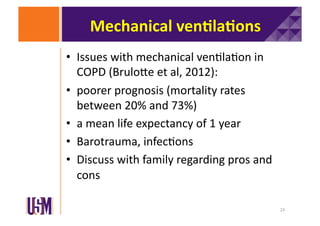
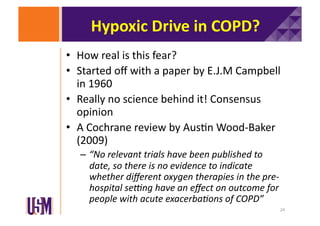
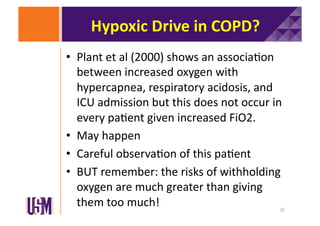
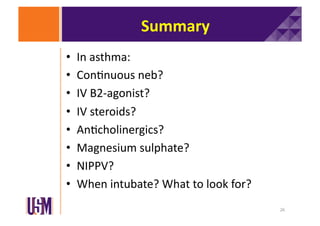
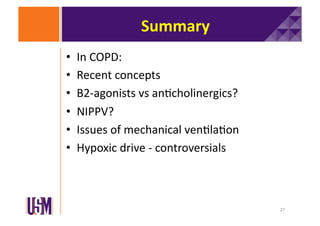
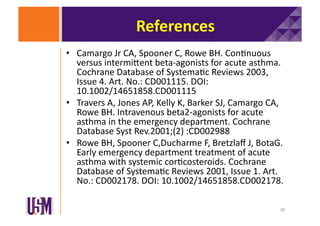
The document discusses updates on asthma and chronic obstructive pulmonary disease (COPD), highlighting key treatments such as continuous nebulization, intravenous beta-2 agonists, and the role of steroids. It emphasizes the importance of recognizing uncontrolled asthma symptoms and the management of COPD through bronchodilators and non-invasive positive pressure ventilation (NIPPV). Additionally, it addresses the controversies surrounding hypoxic drive in COPD and the implications for oxygen therapy in exacerbations.