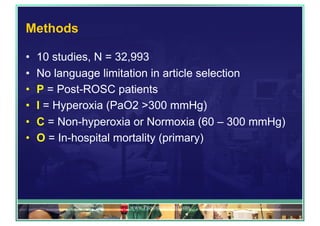
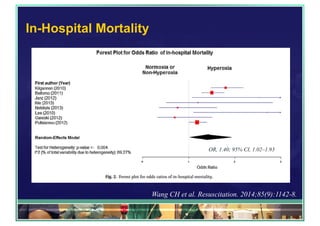
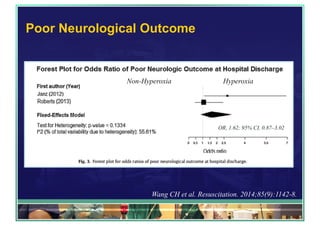
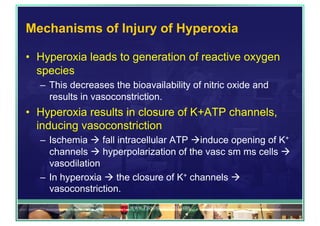
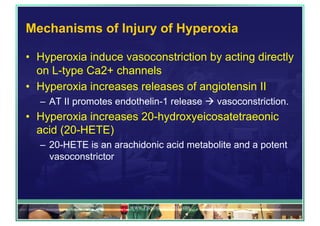
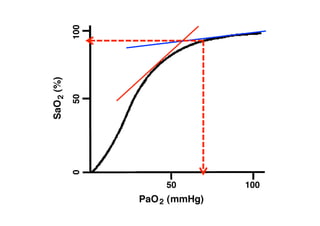
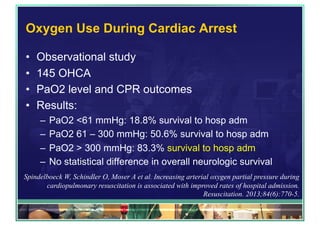
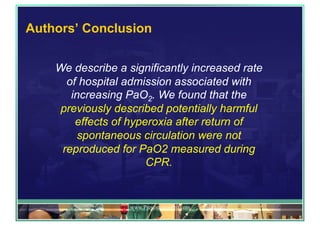
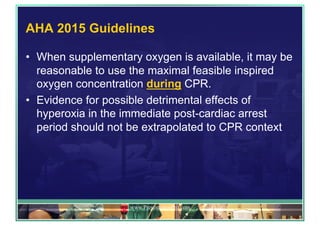
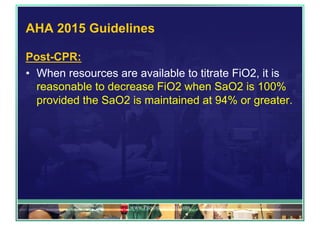
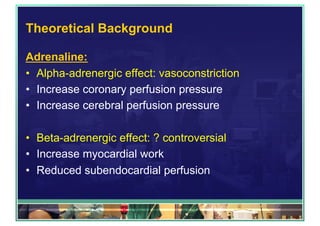
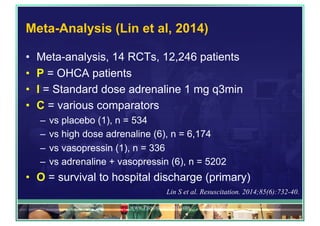
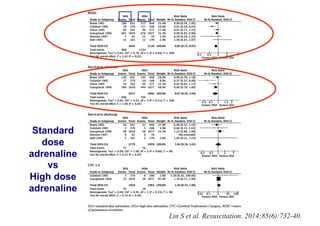
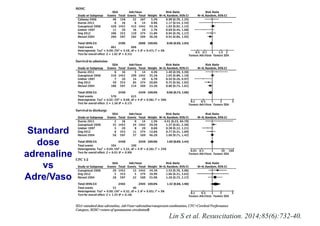
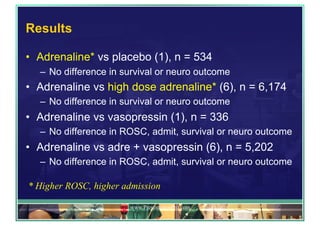
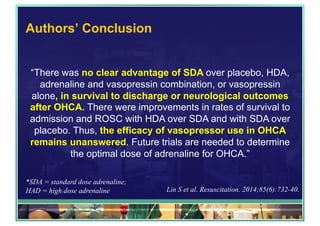
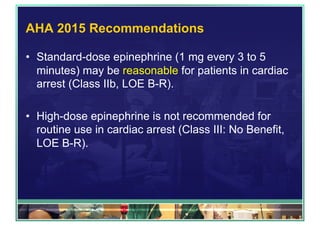
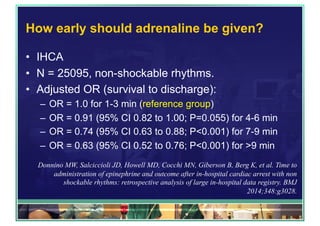
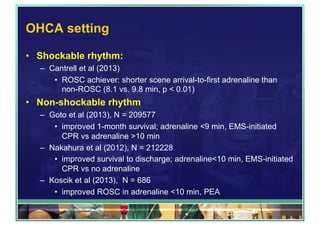
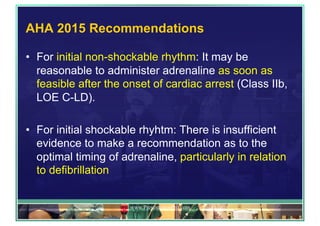
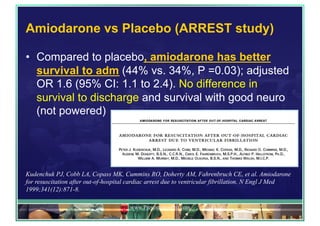
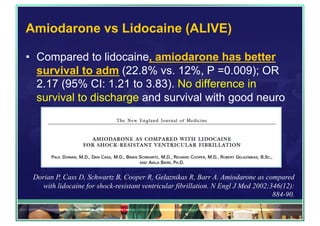
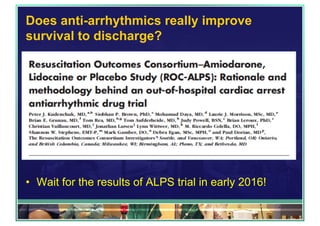
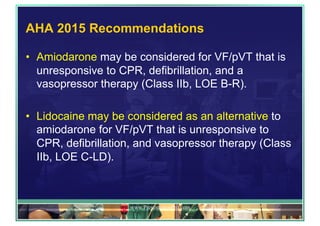
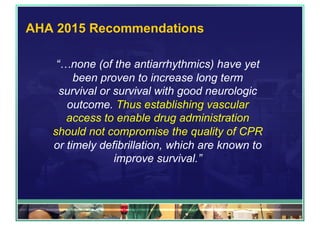
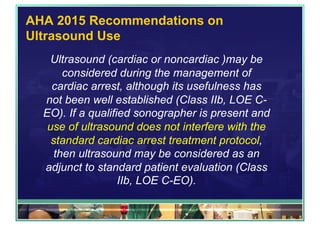
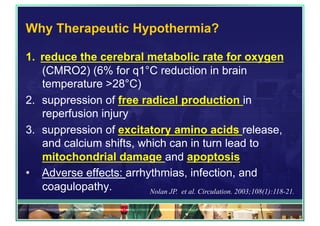
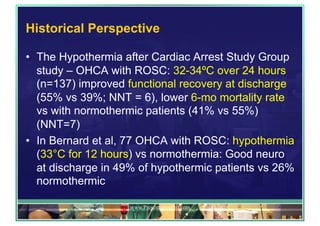
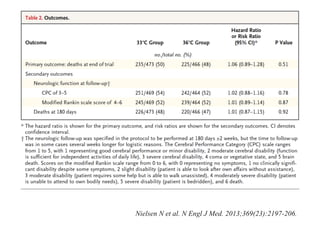
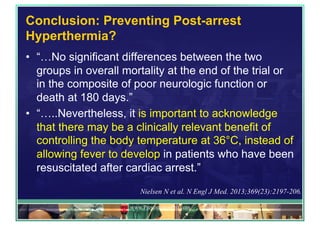
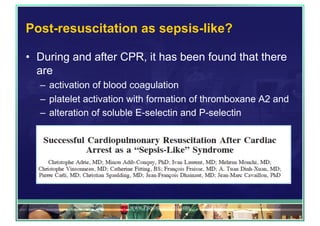
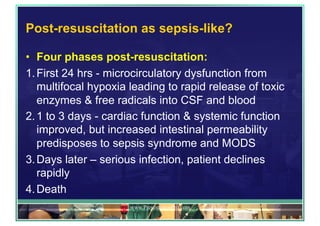
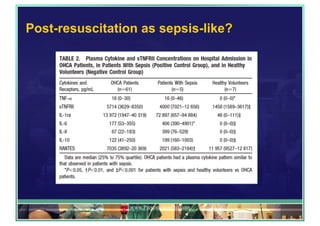
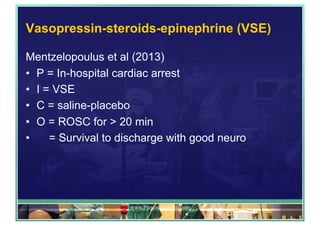
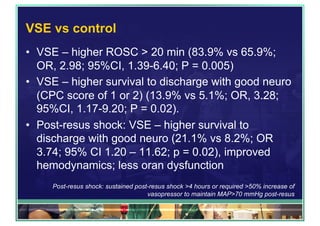
The document outlines updates on advanced cardiac life support in 2015 from a Malaysian perspective, emphasizing the impacts of oxygen use, adrenaline protocols, anti-arrhythmic drugs, therapeutic hypothermia, and potential new therapies involving a combination of adrenaline, vasopressin, and steroids following cardiac arrest. It discusses the evidence supporting the role of oxygen levels during CPR and the effects of adrenaline dosage on survival outcomes, alongside guidelines and meta-analyses relevant to these topics. Additionally, it conveys the significance of managing hyperoxia and the importance of timely intervention in cardiac arrest scenarios.