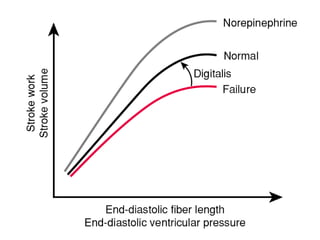
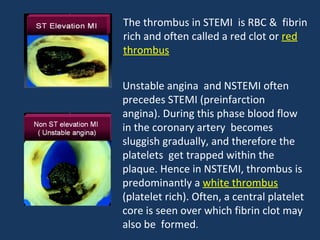
The document provides an intensive review of emergency medicine focusing on cardiovascular physiology, particularly cardiac output and the pathophysiology of acute coronary syndrome (ACS). It discusses the mechanisms involved in the management of ACS, including the role of thromboxane A2 and prostacyclin, the effects of aspirin, and the distinctions between ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina. Additionally, the document addresses related conditions like asthma and chronic obstructive pulmonary disease (COPD), emphasizing the airway inflammation and airflow limitations characteristic of these disorders.