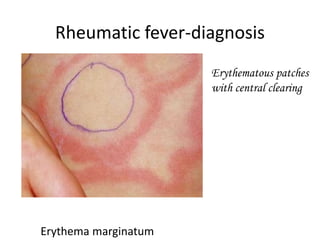
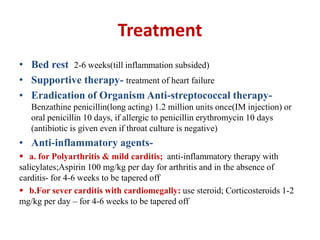
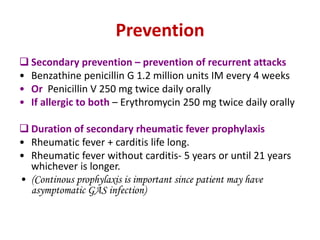
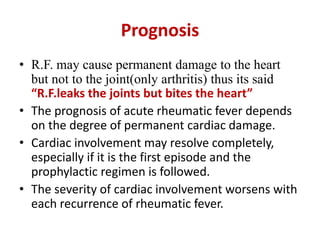
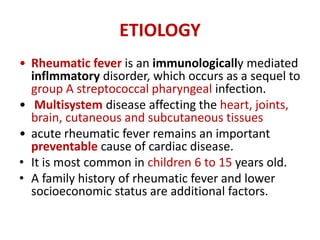
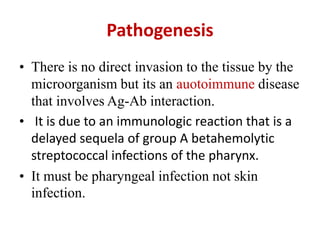
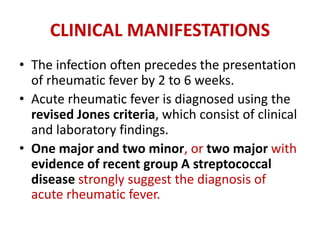
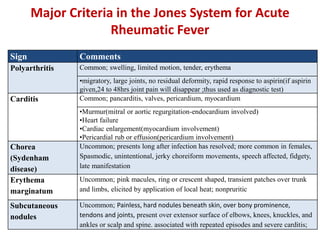
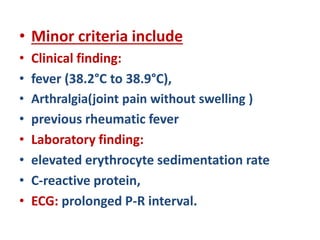
This document discusses rheumatic fever, including its etiology, pathogenesis, clinical manifestations, diagnosis, treatment, prevention, and prognosis. Rheumatic fever is caused by an autoimmune reaction following a Group A streptococcal throat infection. It affects the heart, joints, brain, and skin. Diagnosis is based on clinical criteria including arthritis, heart involvement, chorea, and evidence of a prior streptococcal infection. Treatment involves bed rest, antibiotics to eradicate the infection, and anti-inflammatory drugs. Recurrences can be prevented with long-term antibiotic prophylaxis. Prognosis depends on the degree of cardiac damage, which can sometimes resolve but worsens with repeated episodes.

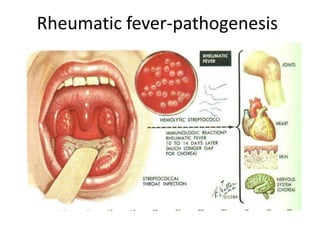
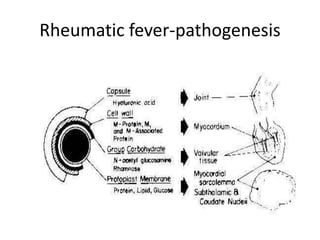
![• Group A streptococcal(GAS) pharyngeal
infection
• Body produce antibodies against streptococci ->
• These antibodies cross react with human tissues
because of the antigenic similarity between
streptococcal components and human connective
tissues (molecular mimicry)[there is certain
amino acid sequence that is similar between GAS
and human tissue]->
• Immunologically mediated inflamation &
damage (autoimmune) to human tissues which
have antigenic similarity with streptococcal
components- like heart, joint, brain connective
tissues.
Pathogenesis](https://image.slidesharecdn.com/rheumaticfever-150329184014-conversion-gate01/85/Rheumatic-fever-6-320.jpg)
![Evidence of recent group A streptococcal
disease
• Supporting evidence for antecedent Group A
streptococcal infection
• scarlet fever,
• Positive throat culture(in 25% of patients )
• Rapid streptococcal antigen test
• Elevated or rising streptococcal antibody titer
– ASO[anti-streptolysin] or Anti DNAseB,
AH[anti-hyoluronic acid])](https://image.slidesharecdn.com/rheumaticfever-150329184014-conversion-gate01/85/Rheumatic-fever-10-320.jpg)