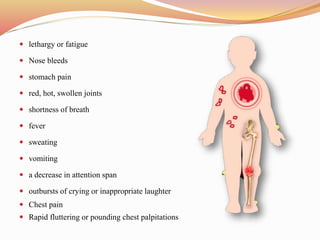
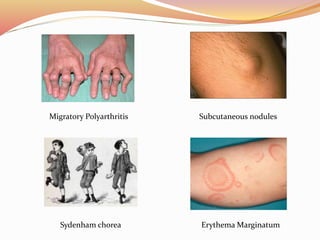
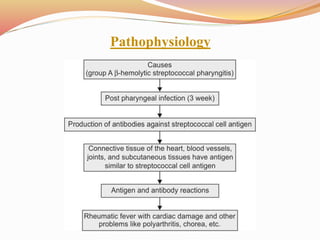
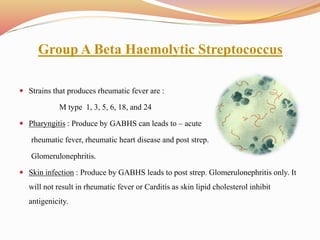
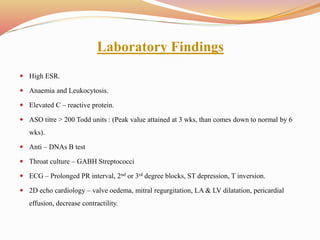
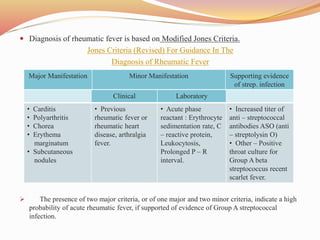
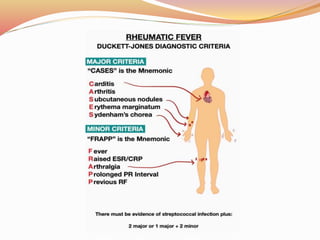
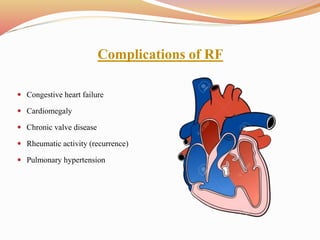
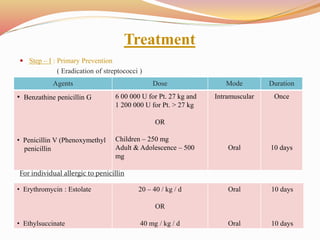
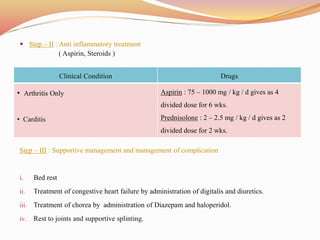
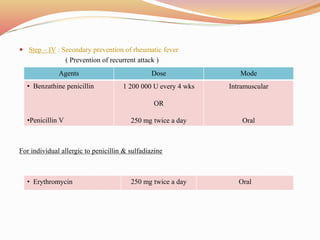
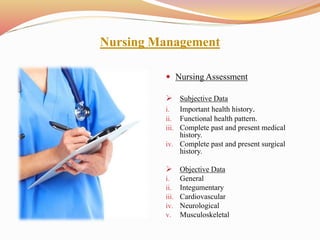
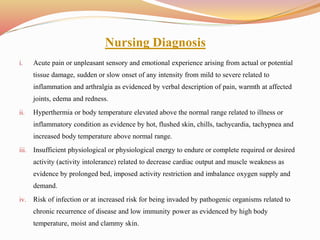
Acute rheumatic fever is an inflammatory disease that can develop following a streptococcal infection such as strep throat or scarlet fever. It primarily affects the heart, joints, brain, and skin. Common symptoms include fever, joint pain, abnormal heart rhythms, involuntary movements, and rashes. It is most common in children ages 5-15. Treatment involves antibiotics to treat the initial infection, medications to reduce inflammation and symptoms, and long-term preventative antibiotics to avoid recurrence. Nursing care focuses on reducing fever, monitoring for cardiac complications, maintaining activity and rest, and educating patients and families.