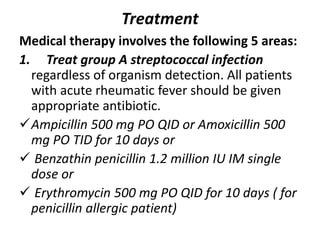
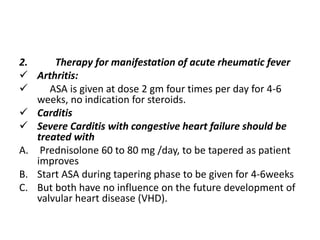
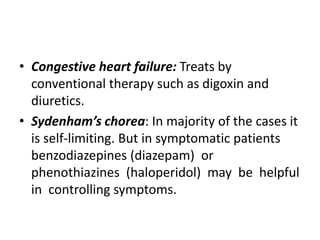
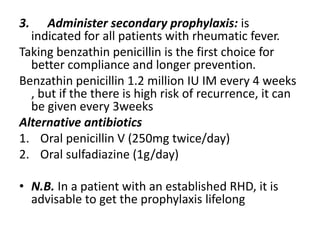
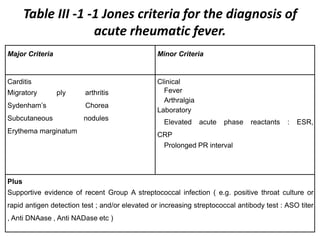
Rheumatic fever is a sequel to group A streptococcal infection, usually of the throat. It causes chronic damage to the heart valves. The Jones criteria are used to diagnose it based on major manifestations like carditis or migratory polyarthritis, and minor criteria like fever or arthritis. Treatment involves antibiotics for the streptococcal infection, aspirin or steroids for inflammation, and lifelong antibiotic prophylaxis to prevent recurrence and further heart damage. Preventing initial streptococcal infections is key to reducing rheumatic fever incidence.
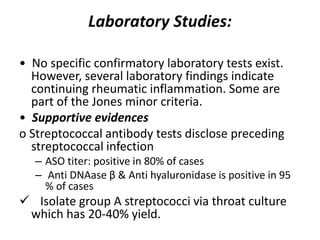
![Laboratory minor criteria
Acute phase reactants (e.g. raised ESR and C-
reactive protein [CRP])
Leukocytosis may be seen.
• Anemia usually is caused by suppression of
erythropoiesis.
• ECG: PR interval prolongation is seen in 25%
of all cases but is neither specific to nor
diagnostic.](https://image.slidesharecdn.com/l1-170220113144/85/L1-rheumatic-fever-14-320.jpg)