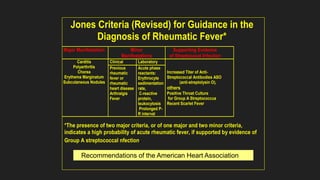
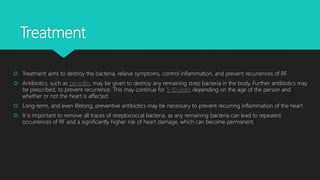
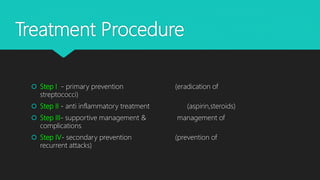
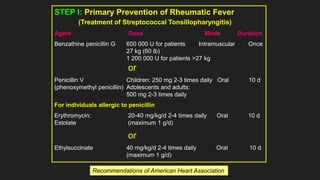
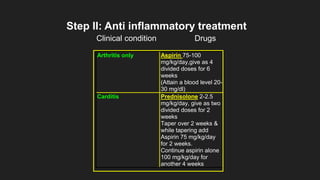
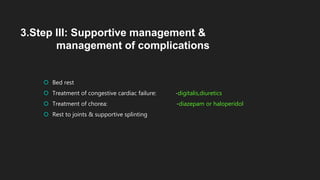
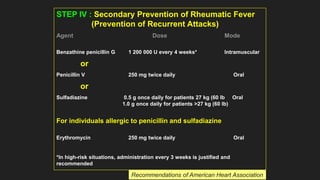
Acute rheumatic fever is an autoimmune disease stemming from group A streptococcal throat infections, primarily affecting children aged 5-15 and can result in serious heart complications if untreated. The condition leads to inflammation in various body systems, with symptoms including joint pain, skin rashes, and potential heart damage. Diagnosis relies on clinical criteria and treatment includes antibiotics to eliminate the bacteria and anti-inflammatory medications to manage symptoms and prevent recurrences.