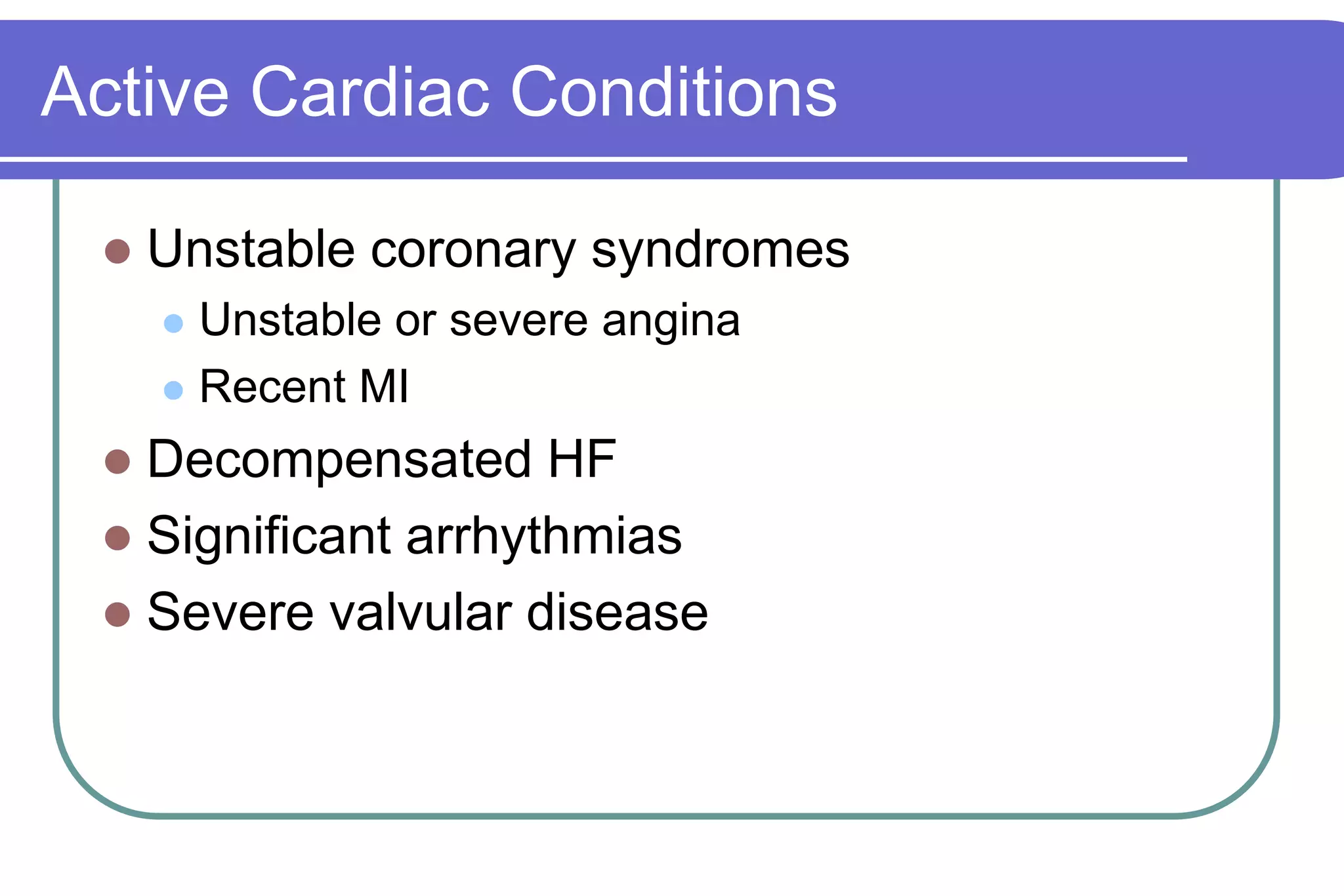
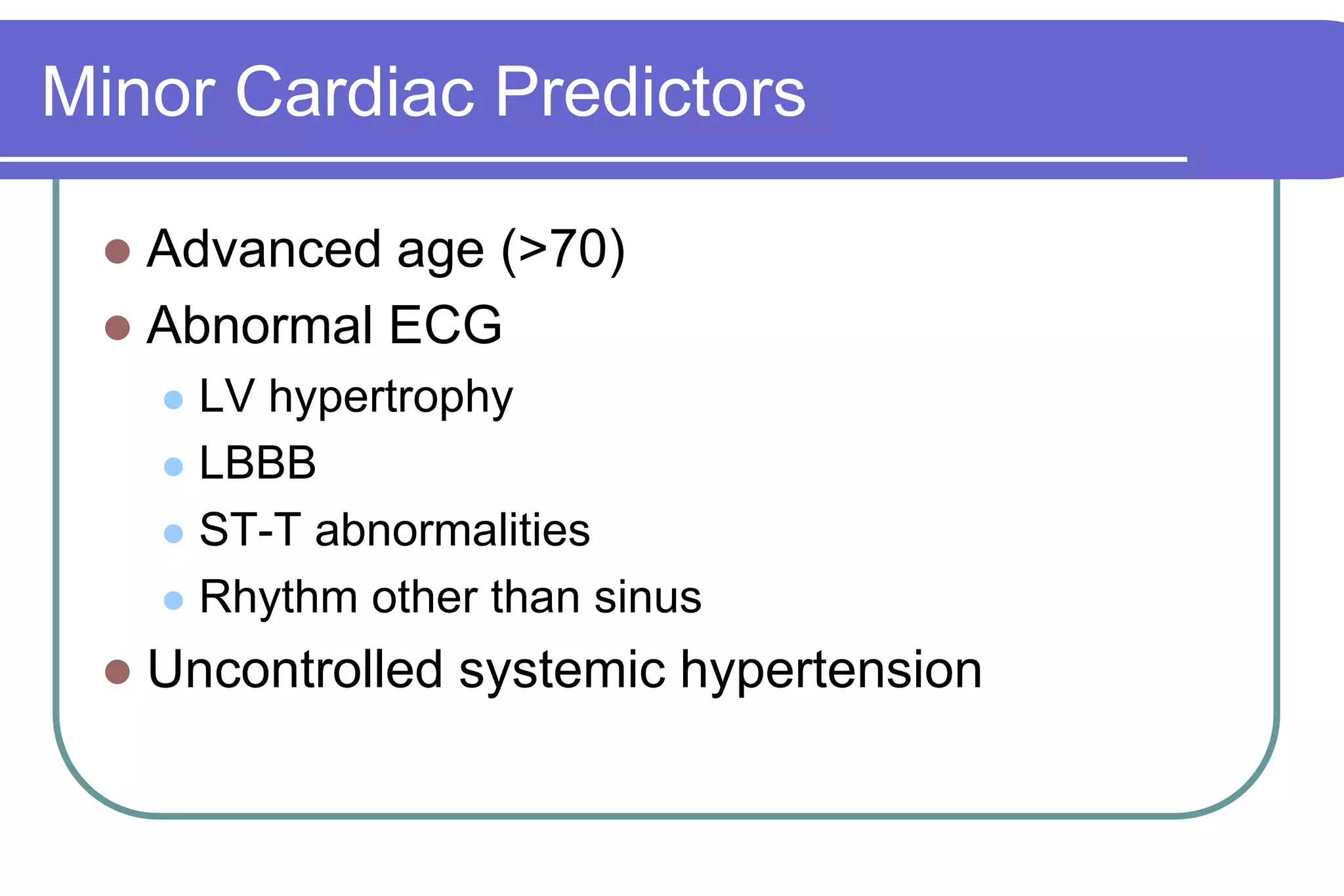
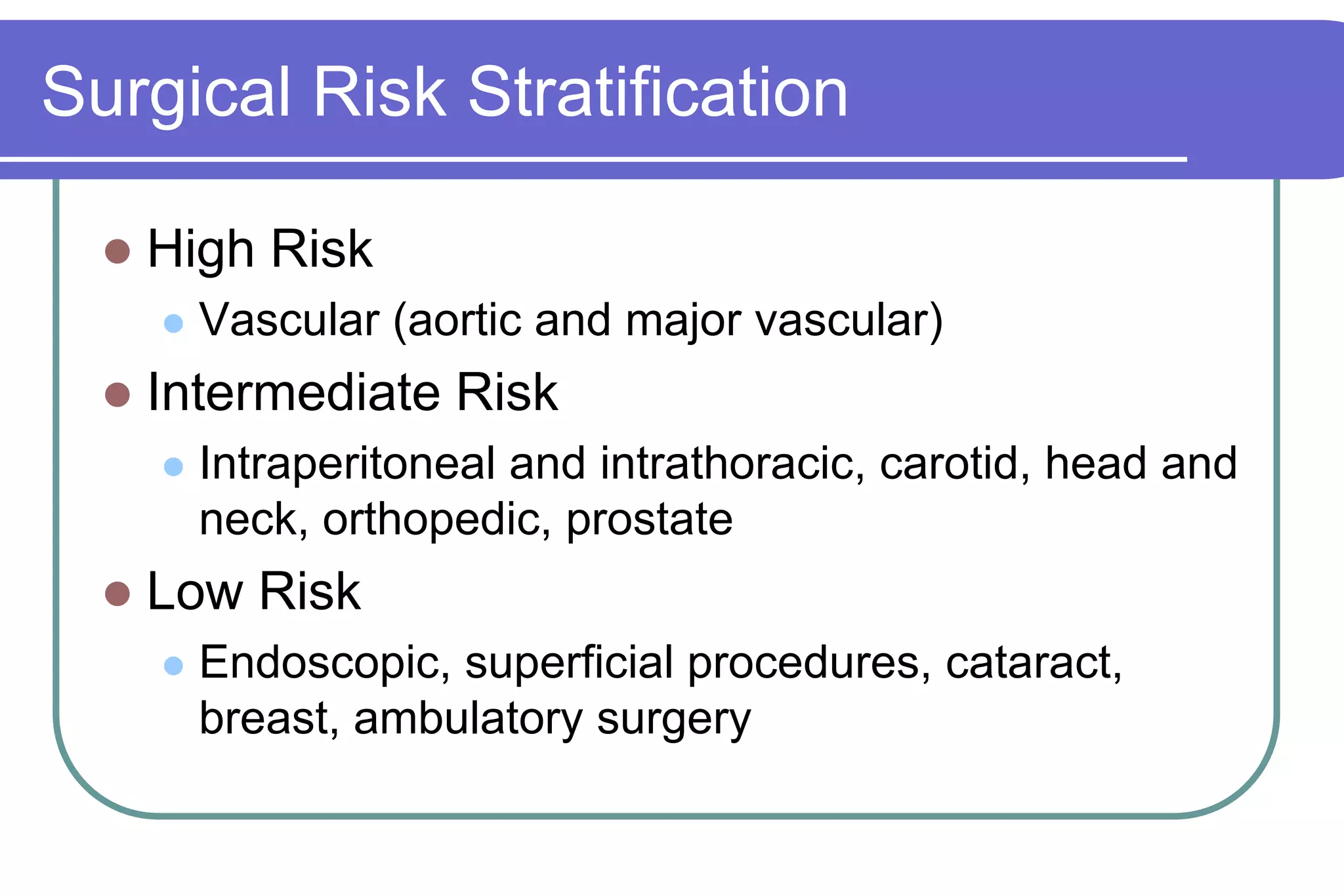
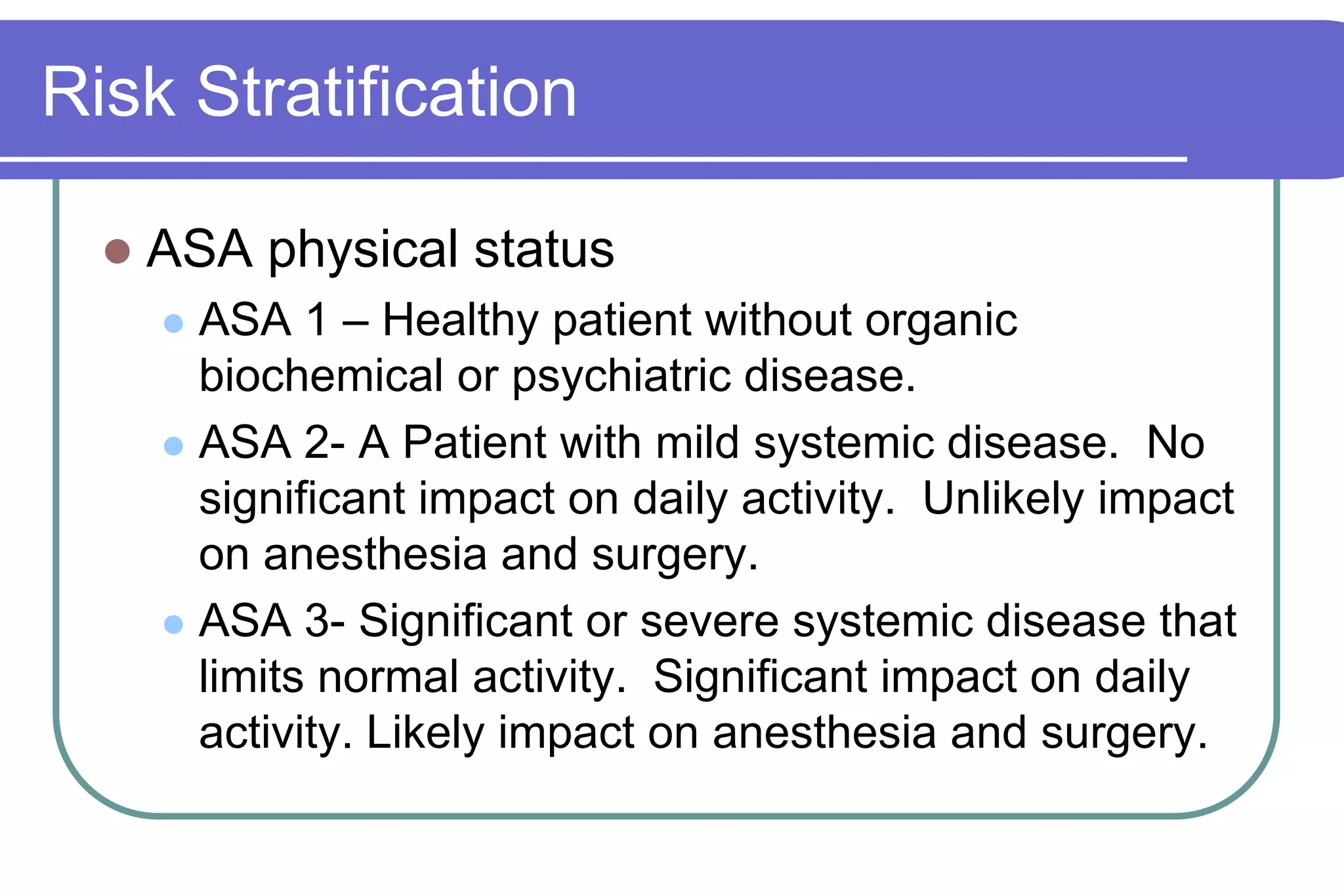
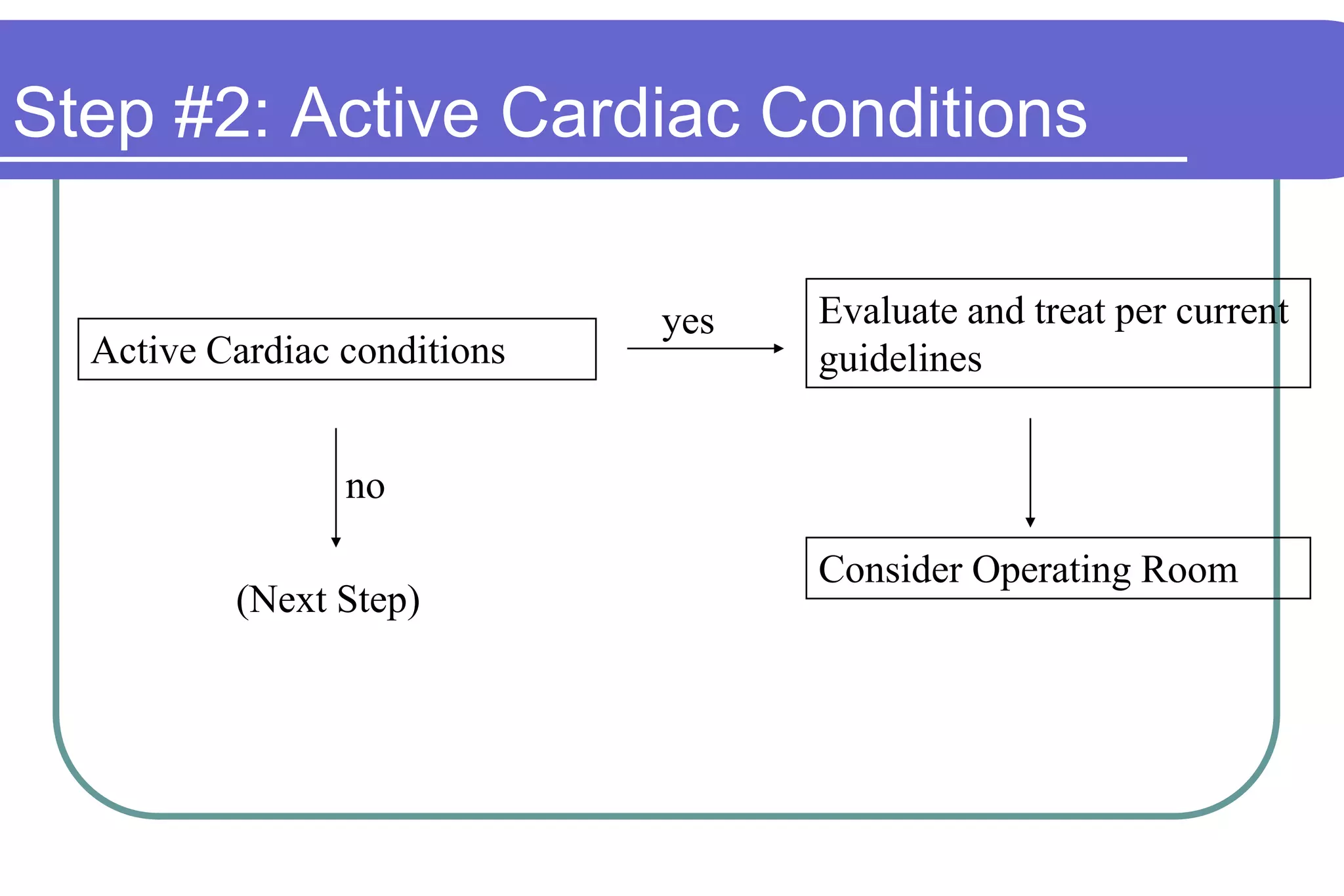
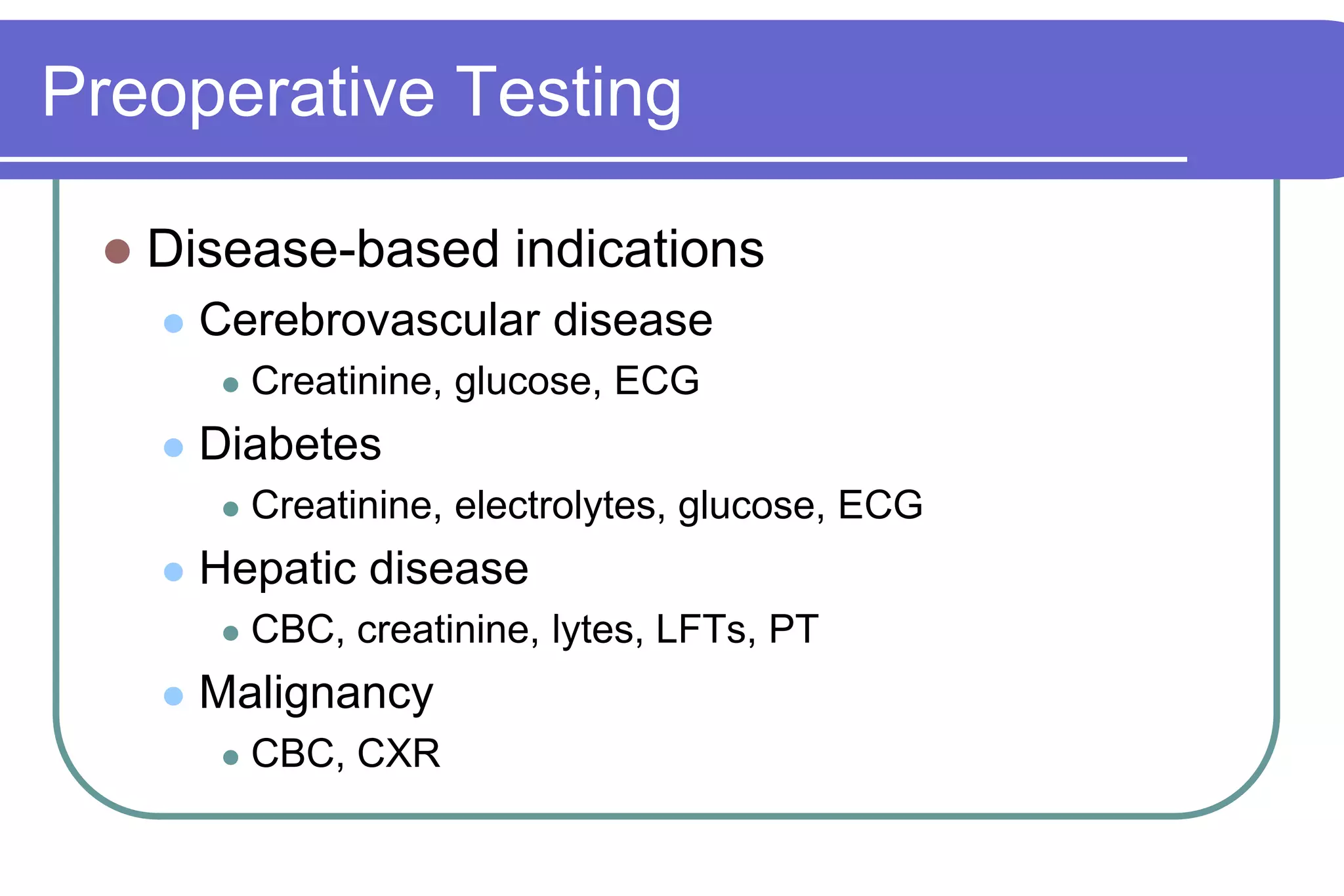
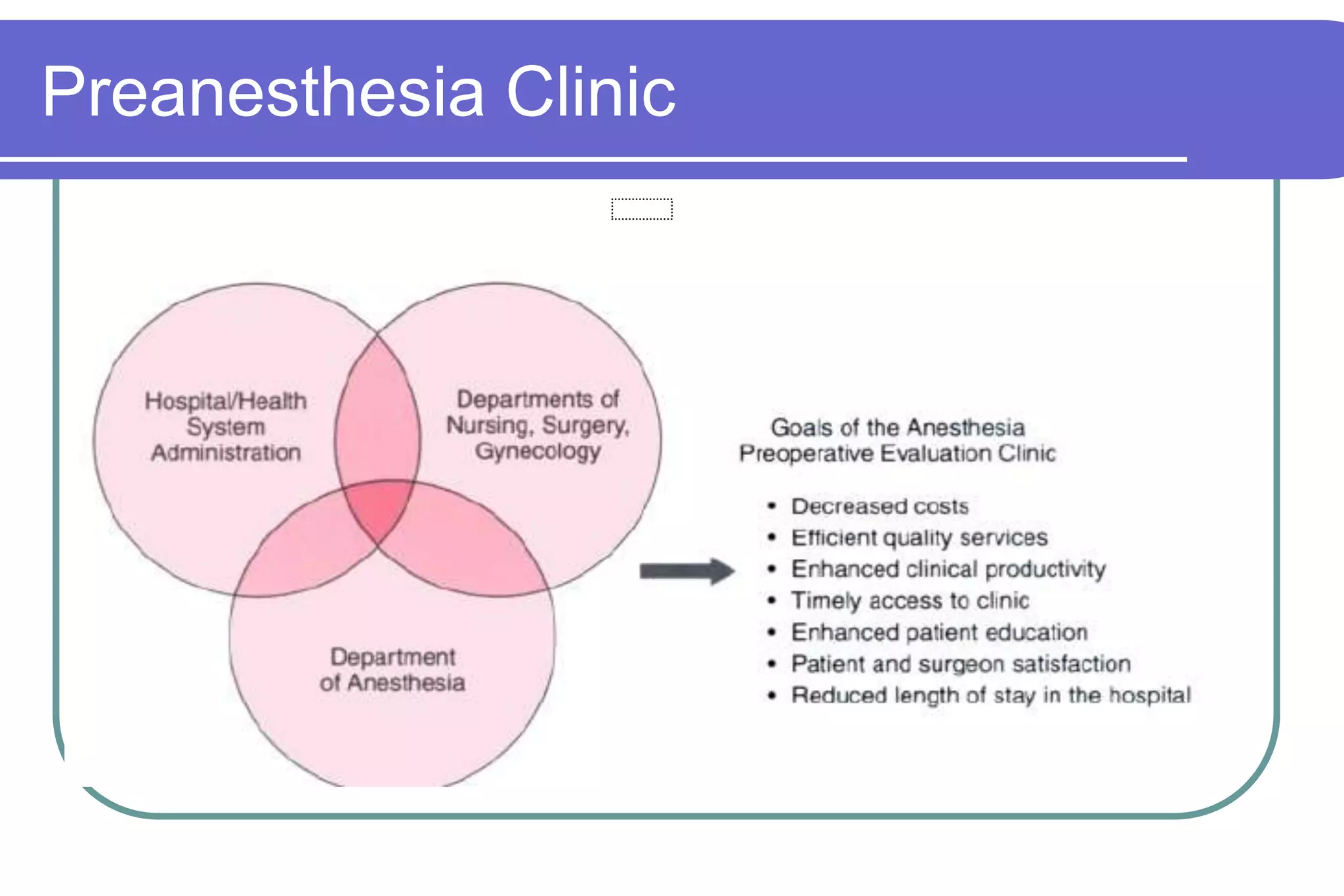
The document outlines the objectives and components of an anesthesia and CPR course for medical students. It covers pre-anesthesia assessment, orientation to anesthesia equipment, post-operative care, ICU rounds, and the role of anesthesiologists in the pre-operative period. Key topics include pre-anesthesia evaluation, anesthesia principles, medical history taking, risk stratification, airway evaluation, preoperative testing, informed consent, and documenting the preoperative visit.