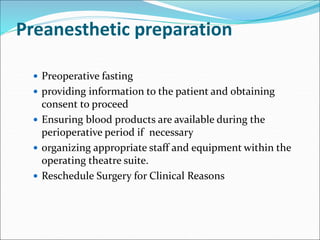
This document outlines the process and importance of preanesthetic evaluation. It defines preanesthetic evaluation as a medical check-up and lab tests done before surgery to assess patient health and risks. The evaluation aims to optimize patient preparation, ensure surgery is realistic, and anticipate problems. It involves taking a medical history, examining the patient, ordering relevant tests, and developing a preoperative plan. Factors like ASA grade and POSSUM score can help predict perioperative risks. The evaluation helps educate patients, organize care, and plan anesthesia to improve surgical outcomes.