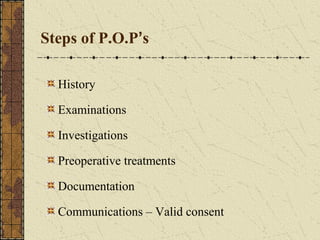
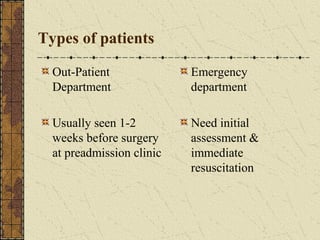
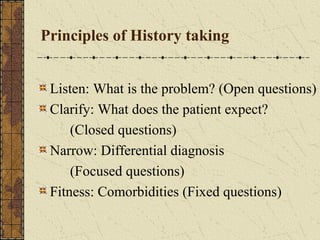
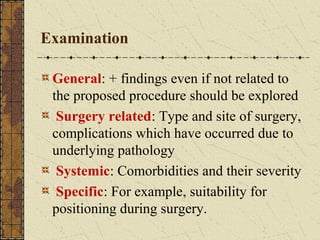
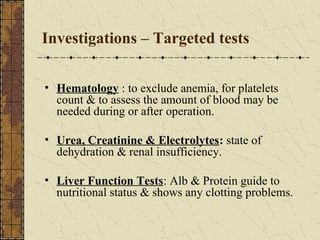
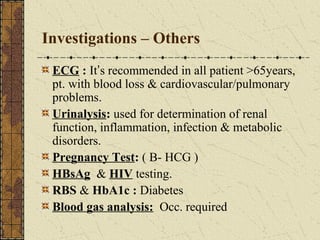
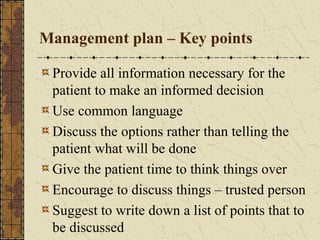
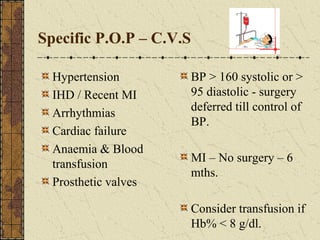
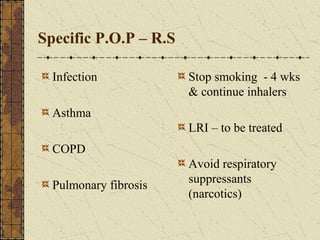
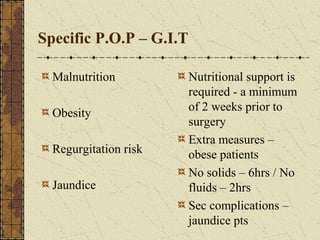
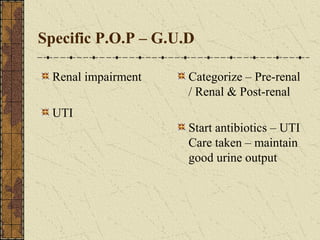
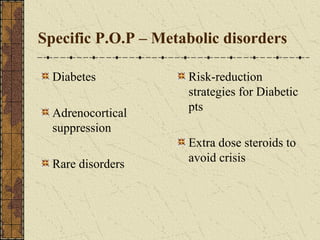
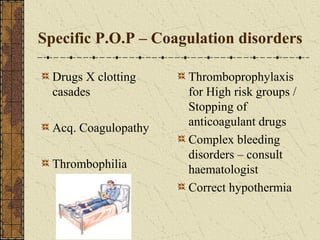
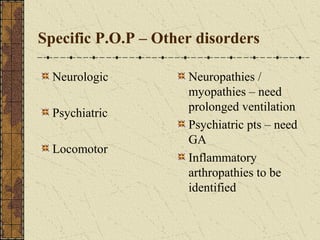
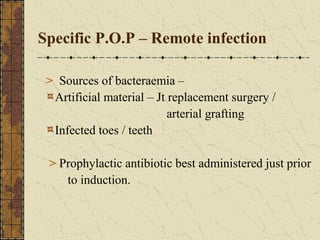
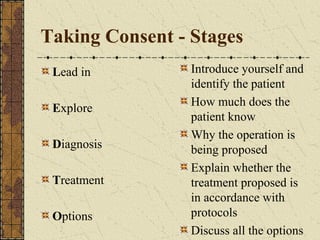
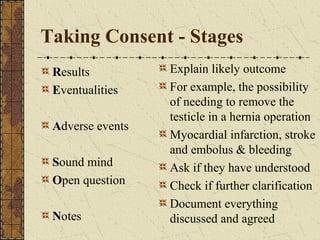
The document outlines the principles and processes involved in pre-operative care, including patient assessment, consent procedures, and specific pre-operative problems. It details the necessary investigations and management plans to optimize patient conditions before surgery, emphasizing the importance of communication and informed decision-making. Additionally, the document highlights various specific patient considerations and complications that may arise during the pre-operative phase.