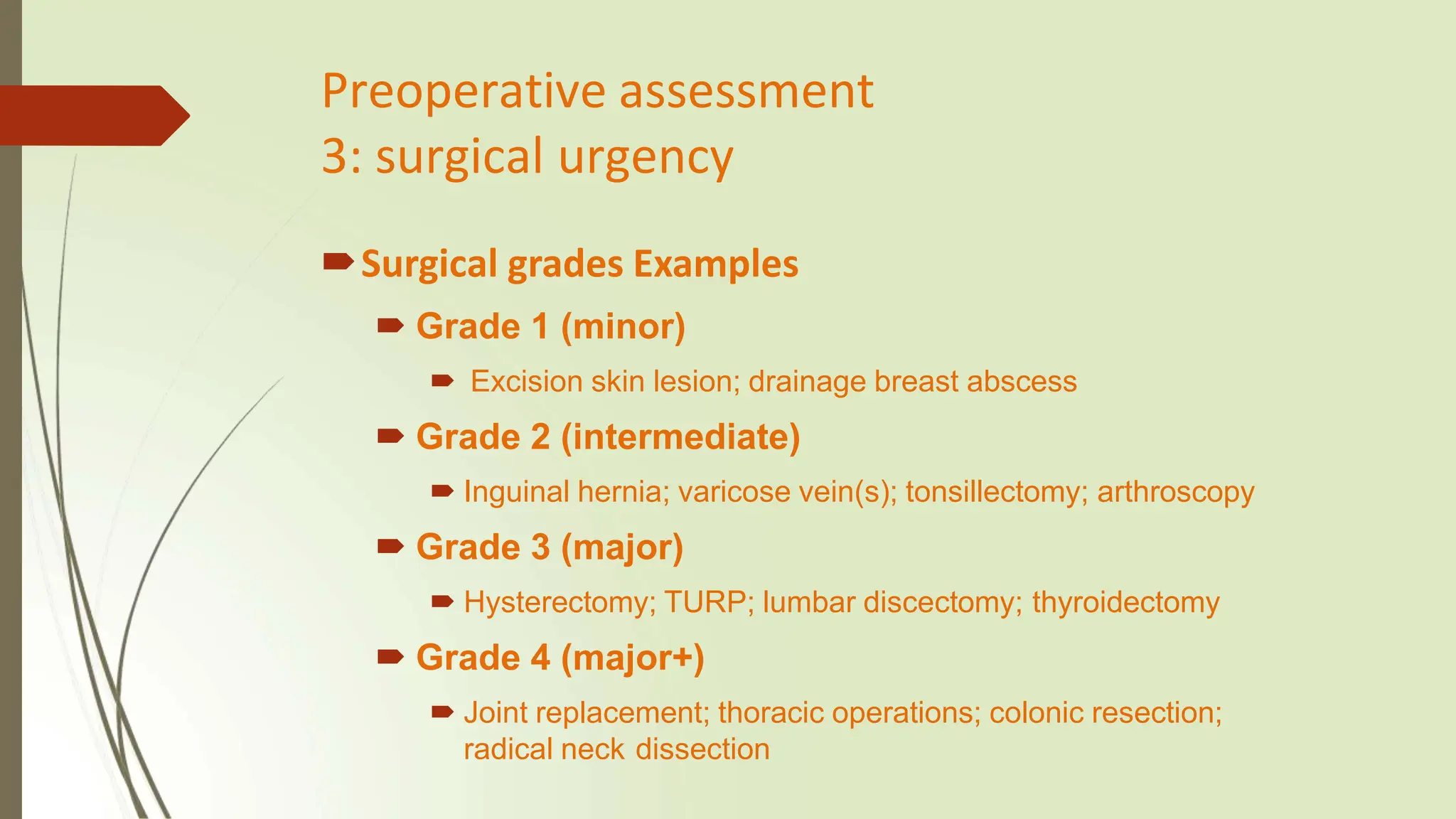
The document outlines the critical components of preoperative assessment and preparation for anesthesia, emphasizing the importance of history taking, physical examinations, and necessary investigations to reduce surgical risks and improve patient outcomes. It details the structured approach to assess patients, including evaluating medical histories, surgical urgencies, and conducting relevant tests such as ECGs and blood counts. The goal of the preoperative assessment is to ensure patients are fully prepared for surgery, minimize complications, and enhance overall surgical management.