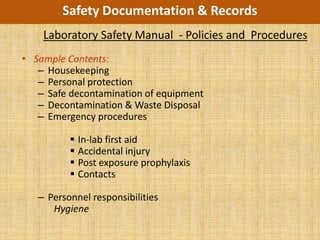
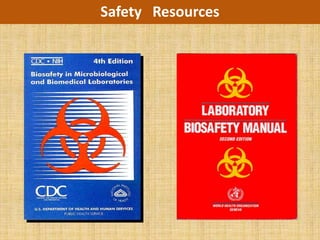
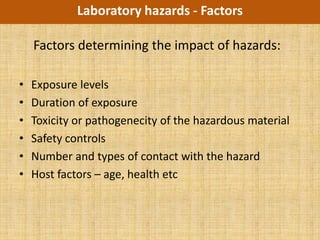
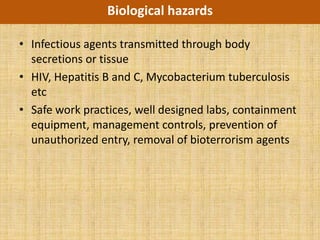
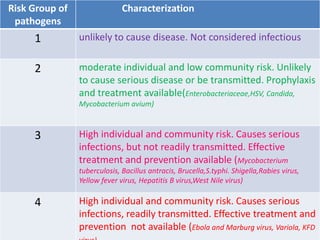
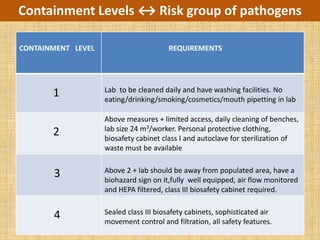
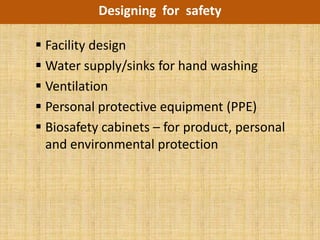
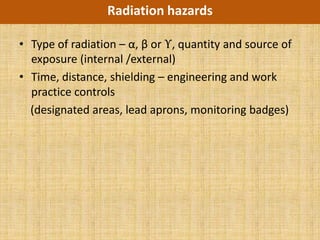
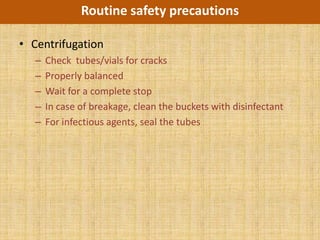
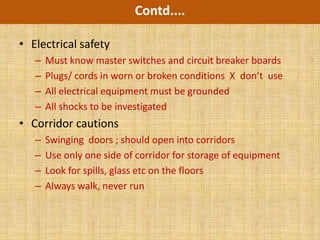
The document outlines the essential components of a laboratory safety program, including identifying biological, chemical, radiological, fire and electrical hazards; developing and implementing safety policies and procedures; and evaluating the program for regulatory compliance to protect workers, products, and the environment from laboratory hazards.